It started with macaroni and cheese. At least that’s the way Kili Cole tells the story.
At age 11, Kili was a healthy girl who loved playing tennis, painting and playing the cello and clarinet. She’s a talented musician with aspirations of attending a performing arts high school and developing a career in music.
And the mac and cheese? Well, after enjoying a bowl, Kili found herself feeling shaky. “I thought it was probably nothing, but my mom wanted to get it checked out,” she said. “After I got tested, it turned out that I have diabetes.”
Type 1 diabetes
Kili has type 1 diabetes, a lifelong condition in which an individual’s pancreas is unable to make a sufficient amount of insulin, leading to high blood sugar levels. Many people with the condition eventually become insulin-dependent, meaning that they have to take daily injections of insulin or use an insulin pump.
Two years later, at age 13, Kili was still able to manage her condition without taking insulin, and she and her family wanted to put off insulin dependency as long as possible. “My doctor, Dr. Edelen, brought up Tzield as a possible treatment during one of my regular appointments,” Kili said.
“She thought Kili would be a good candidate for the treatment,” added her dad, Lance. “But she thought we might have to go to Sioux Falls for it.”
A new treatment
Tzield is a relatively new medication, given through IV infusion, that can help manage type 1 diabetes by delaying the progression of symptoms, including the need for insulin.
“Kili was an excellent candidate for the treatment, because though she was experiencing abnormal blood sugar levels, she wasn’t experiencing any symptoms and she didn’t need insulin,” explained fellowship-trained Pediatric Endocrinologist Rachel Edelen, M.D. “She was in stage 2 of type 1 stage 3, which is where we see patients needing to take insulin. Kili is otherwise a healthy girl.”
Tzield was approved by the FDA in November 2022, but hadn’t been used in Rapid City. Director of Infusion Services Brandi Tackett, PharmD., worked with Dr. Edelen, the pediatric nursing unit at Rapid City Hospital and Provention Bio, a Sanofi Company, the pharmaceutical company that makes Tzield, in order to coordinate making the medication available to Kili.
“Arranging for a new therapy does take some planning and coordination,” Brandi said. “Once we knew there was a patient identified, we worked to assure Kili would be able to get all the necessary infusions as soon as possible.”
Home for the holidays
Tzield is administered over the course of 14 days. Kili received her first infusion on Dec. 12, and she completed her final dose on Christmas Day. “It was a pretty good Christmas present to be done with the infusions,” Kili said with a laugh. “Although it wasn’t too bad.”
The infusion itself doesn’t take too long – roughly thirty minutes. But preparing the treatment added time to each visit, so Kili would spend at least an hour in a hospital room each visit. “The first seven days we were there almost three hours, because they were testing her white blood cell count, and it had to be sent to the lab,” Lance said.
“Then they tested it again I think on the 11th day,” Kili added. “Those were long days, but there were some days when we were only there for about an hour.”
Tzield can cause side effects that include headache, nausea, fever, joint and muscle pain and fatigue, but Kili only experienced fatigue after her infusions.
As far as side effects go, Kili’s experience wasn’t too bad. She experienced fatigue and a little nausea, but she didn’t have many complaints. “Mostly I felt really tired after getting the infusions,” she said. “And I did get sick at the end of the treatment — just a cold, but it made my blood sugar rise. I was so glad to be able to just go home afterward and sleep in my own bed, instead of having to stay in a hotel or something.”
Kili’s blood sugar has since stabilized, and although it has been within the normal range, she will continue to monitor it.
“I think the side effect that we saw the most was just that she was so tired,” said Lance. “We’d take her home and she would go and sleep for a few hours. Being able to do the treatment here was really a blessing, because I don’t think she would have been as comfortable if we were staying in Sioux Falls.”
Kili and her family were grateful that she could receive care close to home, but also for the quality of care she received. The nurses that administered the infusions put Kili at ease and made her as comfortable as she could be during the process. “The nurses were amazing. I don't know how I would have gotten through it without them,” she said. “I remember when they first put my IV in, it was really scary for me, because it was the first one I ever had, but the nurses were singing and dancing the whole time, just to make me smile and not feel so scared about it.”
Tzield isn’t a cure for type 1 diabetes, but it does delay the progression of the condition, most notably the need to take insulin. “Kili was showing signs of moving toward insulin dependency,” said Dr. Edelen. “This treatment will push back her need to use insulin for two years. That’s significant.”
“She’ll be in high school at that point,” added Lance. “And then, who knows what will be available for treatment.”
Type 1 diabetes is a lifelong condition that, until recently, was commonly referred to as juvenile diabetes. It got that name because it often rears its head in children and teens, although people of any age can get it.
When it comes to the cause, it surprises some people to learn that it’s still unclear what causes type 1 diabetes. It’s known that genetics plays a role, and that having a family member with the disease increases the risk, but there is no definitive cause for the condition.
The future
As far as high school and beyond, Kili has big plans. She intends to audition for the University of North Carolina School of the Arts high school program. “I would really like to focus on music for my future career, and it would be great to be able to go there. And graduates can get free tuition for UNC system colleges, so it would be an amazing opportunity,” Kili said.
Tzield has a bright future in Rapid City as well. Now that the groundwork has been laid, it will be much easier for additional patients to have access to the medication. “The relationship has been established, so we’re able to get Tzield as needed. Working to get the medication here for Kili has the added benefit of ensuring that other patients would have access to it as well,” Brandi said.
Her decision to get the treatment, and to do it in Rapid City instead of traveling to Sioux Falls, has opened the door for other patients to get the treatment, especially those who may not be able to travel to the other side of the state and stay for two weeks. “It feels nice to know that it isn’t just helping me, but will help other people too,” Kili said. “I’m glad I did it, but it was a long process and I was happy that I could go home after each session. I’m glad that it’s also available now to someone else who might need it.”
Story by Wade Ellett
Photos by Bob Slocum
When did you first learn the truth about Santa Claus? No, not that truth. The one about Santa’s network of helpers around the world who help him make holiday wishes come true for millions of girls and boys. After all, it’s a big job, and even with a sleigh full of Christmas magic, Santa needs all the help he can get. Dana Darger, RPh, Director of Pharmacy at Rapid City Hospital knows firsthand just how hard Santa’s job can be. There’s hours of work to do, often in the cold, but nobody would ever say it’s a thankless job. “I think being Santa is one of the most gratifying experiences a person could have,” said Dana. “There’s something about Christmas and Santa that helps kids believe in magic.”
“And it makes adults feel like little kids again,” he added with a chuckle.
So how exactly does Dana know about the hard work that Santa Claus puts in? It’s simple — he is Santa Claus. Okay, maybe he’s not The Santa Claus — his driver’s license doesn’t say Kris Kringle, and he doesn’t live at the North Pole — but he’s one of a select few people in the world who have the honor of putting on the red suit and becoming Santa for children of all ages.
Before the suit
It takes more than just putting on a costume to make a person Santa Claus. Sure, anyone can stuff a pillow down their coat and throw on a fake beard, but it won’t take long for kids to see through it. No, there’s more to being Santa than just a fancy costume. It starts with the Christmas spirit, and that starts with a giving heart.
“You know, when my wife and I first got married we were both in college, so we were pretty poor. We made all of our Christmas presents,” Dana shared. A lot has changed since then, and the Dargers are no strangers to buying gifts, but Dana still enjoys making them — a fact that his pharmacy staff could attest to. “When I'm making gifts for someone, I pray for that person and meditate on that person. I'm trying to put them and myself into that gift. I think that’s how Santa makes presents,” Dana said. “I don’t know if I can tell you exactly when I figured out Santa had helpers all over the world, but that’s part of the magic of Christmas. You just have to have a giving heart.”
Making gifts? Check! A giving heart? Check! Throw in his happy, childlike demeanor, positive attitude and white beard, and Dana Darger had all the right stuff to become Santa Claus. All that was missing was that one little nudge toward the red suit — and to learn where that nudge came from, you need to get to know Denny Leibel.
Partners in shine
Denny Leibel, Pharmacy Business Analyst, works closely with Dana at Rapid City Hospital. Like Dana, he shares a love of Christmas magic, and for him that magic means one thing in particular: lights!
“When I was a kid I was always fascinated with Christmas lights. I remember driving around looking at houses where people had a display and it always brought me joy. Those are. memories I cherish,” Denny said. “So a long time ago, I thought that my ultimate goal was to have that ‘go-to house’ that everybody wanted to go see. I think we've accomplished that for sure.”
Denny isn’t mistaken — for the past 15 years he and his family have put up holiday displays to celebrate the season. “We started small, but for the last five or six years, we’ve exploded.” That’s not an exaggeration. An explosion of light is exactly what you’ll get when you pay his house a visit during the holiday months, but it isn’t a chaotic scene. Quite the opposite, in fact — the entire display is coordinated and organized, from illuminated snowmen to a blinking light show synchronized to Christmas music. Think “National Lampoon’s Christmas Vacation,” but with a much better eye for design.
“My wife is the designer and is truly the mastermind at instructing me where things go,” Denny explained. “We’ve got to get things in the right place, and we’ll look at pictures from the year before and put things back where they were if it worked well, or move them if it was a bad spot for them. The first couple of days are the hardest, and it takes a few weeks from start to finish.”
It’s a big endeavor that involves large decorations like a 7-foot illuminated Santa, giant snowmen, hundreds of extension cords, and waterproofing junction boxes. Denny and his family think of Christmas all year round — from dreaming up new features for the display to fixing anything that has broken in the previous season, the Leibels always have the holidays on their minds.
“Sometimes people ask me why we do it, and honestly it’s because I enjoy it,” Denny said. “I love seeing the kids get excited about it. A lot of people think about their lives and wonder what their legacy will be. I guess if my legacy is that I put up a big Christmas display, and created a lot of smiles, I’m happy with that. I can do Christmas.” The centerpiece of the Christmas display is Santa’s chair, where you’ll find Dana, decked out in his red suit, every Friday and Saturday night until Christmas.
Becoming Santa
Dana had all the makings of a great Santa Claus. All he needed was the little push to get him to put on the suit.
It turns out, it was Denny adding Santa’s chair to his winter wonderland that sealed the deal.
“Denny bought the chair after Christmas — it was part of a store’s holiday display — and I asked him what the heck he was going to do with it. Of course he was going to put it in his yard the following Christmas,” Dana said with a chuckle. “I teased him about it for a couple of months, telling him that you can’t have the chair without Santa sitting in it. Then one day I walked past his desk and said, ‘If you’re not going to be Santa, can I?’”
Just like that, it happened — it was all over except for getting the suit. “Honestly I was just teasing him, but something about it resonated with me. It was something that I truly wanted to do.” And if he was going to do it, he was dedicated to doing it right. He had no interest in a cheap Santa suit, many of which were easy enough to find online. “The nicer suits were more expensive, which I had no problem with,” he said, “but I didn’t want to order one and have it arrive only to find it was no good.”
By this time, it was October, and Santa suits were not really a hot commodity. If you’re going to be Santa Claus, however, you can’t be easily deterred. During a family visit to Denver, Dana took some time to visit a costume shop.
“They were in full Halloween mode, but had one Santa suit on the rack. There was just no way it was going to fit, and it wasn’t really what I was looking for,” Dana said. The proprietor suggested that he return after Halloween. “When I told him where I live and that I couldn’t make it back, he asked me to wait a minute. When he came back, he told me, ‘They’re bringing a rack of suits over from the warehouse,’ and not long after they wheeled in a rack with probably 50 suits on it.”
Looking through the rack, Dana found the perfect suit — it was one of the pricier suits he had looked at online, and it was a near-perfect fit. “It’s like it was meant to be. I had already been letting my beard grow out, now I had the suit, and that was my first Christmas at Denny’s,” Dana said.
‘You can’t play Santa’
A little lighthearted teasing between friends had led to something magical, but Dana still had his work cut out for him. After all, if it was easy to be Santa Claus, everyone would do it. “It wasn’t until that first night when I sat down in that chair that I realized that as soon as you put that suit on, you can’t play Santa. You have to be Santa,” Dana explained. It’s his goal to have every kid walk away with hope that they’ll get the Christmas gift that they’ve asked for, but he can’t make any promises. After all, the gift list stays at the North Pole — and Dana has no way to know what parents may or may not be able to get for a child.
“There’s a sacred trust between the kids and Santa. You can’t lie to them, you can’t make something up,” Dana said. “My goal is always to be as real as possible with them, but to give them hope and to help them believe in the magic of Christmas.”
Take for example the girl who asked for a real unicorn — a difficult ask, most would agree. Yet, it would be a shame for Santa Claus to dismiss the girl’s request. After all, if Santa is real, why shouldn’t unicorns exist as well? Dana knew what to do. “I looked at her and I said, ‘You know what, I haven’t seen a unicorn in probably the last 30 years, but if I find one, I'll bring him to your house.’ I wanted to give just a little touch of reality but without destroying hope. I was able to tell her that she probably wasn’t going to get a unicorn, but she could have a little bit of hope that there was some small chance,” Dana explained, “And she walked away believing that there could still be unicorns out there somewhere.”
The Christmas Spirit
It’s been six years since Dana first became Santa Claus, and it has lost none of its joy. For he and Denny, that’s what this is all about — creating a little spark of happiness that kids can carry away with them. “People have asked me if I take donations. I always say no. I don’t want anyone’s money,” Denny said. “I want their smiles. I want them to make memories. People tell me that their new family tradition is coming to my house to see Santa Claus. And if you see how the kids react to Santa, it makes all the work we put into it worthwhile.”
Dana agreed. “Santa can’t guarantee that every boy and girl will get what they asked for, but he can make sure that they walk away with a smile and feeling like I really listened to them, and that I care about them,” he said. “I can spread a little happiness and joy, and I think that’s more meaningful than we grown-ups realize sometimes.”
Regardless of your background, culture or beliefs, Dana and Denny believe that there’s a magic to the holiday season that belongs to everyone. The two have conspired to bring Christmas to life in the Black Hills in a way that makes children and adults repeat a phrase reminiscent of “Miracle on 34th Street.”
“I believe in Santa Claus.”
Ready to pay Santa a visit?
Head to Denny’s house and check out the Christmas lights any night this holiday season.
Santa will be in attendance every Friday and Saturday night from 6-8 p.m. until Christmas. Bring your smiles, and you’ll get a little holiday magic in return.
You’ll find the amazing display at 4311 Paddock Court in Rapid City.
Santa can’t wait to see you there.
Written by Wade Ellett
Photos by Bob Slocum
Homelessness is a serious problem among America’s veteran population. Veterans make up roughly 11 percent of the country’s homeless population. Around 60,000 veterans can be found sleeping on the streets on any given night, and women make up the fastest-growing group among the homeless veteran population.
“There are a lot of reasons why this number is growing,” said Kaylan Harrington, an Emergency Department Technician at Monument Health Rapid City Hospital. “A lot of women veterans are not utilizing VA health care right now either. Many think they don’t deserve it. Others had a terrible experience in the military and they kind of want to separate themselves from that.”
Kaylan is no stranger to military service. She served for 21 years, starting in the Air Force then crossing over to the Army as an officer. She has been deployed six times, with four tours to Iraq and Afghanistan. She now serves in the South Dakota National Guard and attends nursing school at SDSU.
“I have kind of an unusual resume,” she said with a smile, describing the many jobs she’s done in the military. In her most recent tours to Afghanistan, she worked with female engagement teams, who interact with Afghan women — it’s taboo for Afghan women to interact with men who aren’t direct members of their family. She also worked as a prison interrogator in Iraq and as an intelligence analyst. In other words, Kaylan is a legitimate, certified badass. She’s got a quick wit, a sharply intelligent mind, a can-do attitude and a beautiful, friendly smile. For all those reasons, it’s no surprise that she was also the first runner-up in the 2022 Ms. Veteran America competition.

“I’ve been really humbled by all of this. I’m kind of a tomboy, a T-shirt and jeans kind of girl, and I thought this was something that I couldn’t do,” she said warmly. “But I know women who have competed and won, and I was so inspired by what they were able to do, the money they raised for women veterans and the representation that they brought forward on the national stage. I decided this is the year to do it, and South Dakota is a great state to represent. We take care of our veterans, and I would love to see this attitude and the care and compassion that we have in this state become the norm.”
The Ms. Veteran America competition was created in 2011 by Final Salute Inc., an organization with the mission to provide homeless women veterans and their children with safe and suitable housing. The competition supports the organization’s mission in two ways: all proceeds from the event are used to provide housing, and the event itself serves as a platform to build awareness. Fundraising is part of the competition itself. “All the girls worked their butts off for six months to a year to raise funds for the organization, and then all of the ticket sales were added to that,” Kaylan explained. “We raised over $700,000 for Final Salute.” Additionally, the winner and runners-up serve on an advocacy board to continue building awareness of the challenges faced by women veterans.
“I’m very honored to be part of this. I’m humbled. The women that I met are just unbelievable. There were doctors and lawyers right next to tank commanders and machine gunners,”
Kaylan said. “There’s just a wide array of very educated, very humble, incredibly strong women.” Kaylan said her experience in the military has been positive, but she’s aware that hasn’t been the case for every woman who has served. “A lot of women have had very bad experiences, and that contributes to the problems and troubles they experience after they leave the military,” she said. “Women deal with combat differently, they experience PTSD differently. Sexual trauma is a huge issue in the military right now, and the VA was behind the curve when it came to providing resources catering to female veterans that were homeless.”
A lot of homeless women veterans are also single mothers, which presents additional challenges. Kaylan said, “Many shelters may not be safe for children, and male children that are teenagers may be separated from their mom and placed on a side of the shelter just for men, so many of these individuals avoid the traditional shelters.”
Jathe “Jas” Boothe founded Final Salute, Inc., because she discovered there simply weren’t existing programs to help female veterans with children. In 2005, while Jas was in the Army Reserves, she had to deal with a devastating cancer diagnosis only one month after losing everything she owned to Hurricane Katrina. That experience was eye-opening for her, and was ultimately what led her to start Final Salute, Inc. Since then, the organization has helped more than 7,000 women veterans and their children.

Kaylan, as first runner-up, joined second runner-up Ann Lutz, and winner Liliana “Joie” Byrd, as part of an advocacy board that will continue working to bring attention to the problems faced by women veterans, especially homelessness. “One thing that we’ve done is the Bataan Memorial Death March on March 17,” she said. This 26.2 mile march through the desert at White Sands Missile Range in New Mexico is an annual commemoration of the Bataan Death March attended by many survivors, veterans and supporters from across the globe. The trio wore their military uniforms, as well as their crowns and sashes, and raised money and awareness for Final Salute during the March.
“It’s the first time the Ms. Veteran America court has done something like that,” Kaylan said. “So we made a little bit of history, which felt great since it was also Women’s History Month.” Marching through the desert did nothing to deter Kaylan’s excitement for bringing awareness to the plight of homeless female veterans. “I’m excited for everything that we’re planning.”
Final Salute’s mission inspired Kaylan to step out of her comfort zone and onto the stage to compete for Ms. Veteran America, but there was an added bonus. “To bring national attention to this problem is incredibly important, and I’m proud to be part of it. But it also has been a great reminder that women do incredible things in different ways, and you can do more than one,” she said with a smile. “You can be a badass in the military and still want to put on a dress and a nice pair of heels once in a while. One doesn’t have to overshadow the other.”
“This year, the talent portion was a lip sync battle,” said Kaylan with a laugh. “I lip synced Prince’s ‘Let’s Go Crazy’ — I love him, he makes me so happy, and I got really into it. There was a full costume, and I bedazzled my Guitar Hero guitar. I won best talent for the competition.” Kaylan also won most donations, raising $11,000 in South Dakota, all of which will be used to benefit homeless women veterans.
The final day is the evening gown event and the pushup competition. In addition to the judges’ scores, Ms. Veteran America and Final Salute, Inc., leadership also consider contestant activity, interaction and participation.
“I ended up having a lot of fun during the competition, and I’m proud of the work we’re doing to help homeless women veterans,” Kaylan said. “It’s a big problem, but I’m proud to be part of a group that is working on solutions.”
Written by Wade Ellett
Photography by Bob Slocum
In 2016, Laura Brunmaier decided to make a big change in her life. She left a successful and lucrative career in upper retail management and returned to school to finish her degree. “The standard of living was nice,” she explained with a chuckle. “But there wasn’t a lot of meaning behind it for me. I wanted to do something — more.”
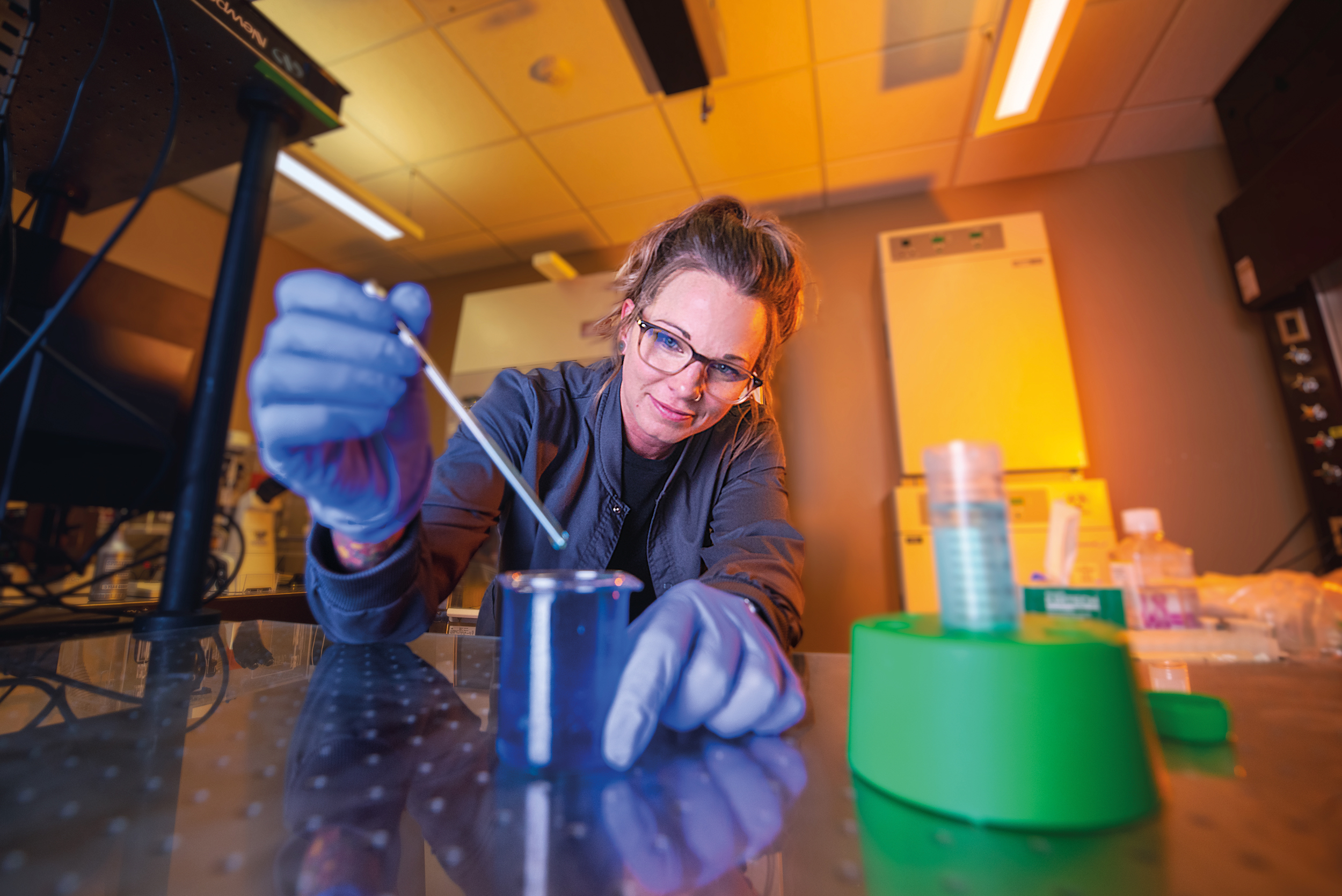
Laura returned to school at SD Mines in Rapid City. Before she even completed her bachelor’s degree in applied biological science, she dove into biological engineering research projects, beginning with nanoengineering. In December 2018, she was introduced to Travis Walker, Ph.D., Associate Professor of Chemical and Biological Engineering, who was looking for a biomedical engineering graduate student to take on a project for making a vascular graft.
“I ended up leaving nano to start in Dr. Walker’s lab about six months before I finished my bachelor’s degree in May 2019. It was a head start on my Ph.D. work,” Laura said. “I knew we were making this vascular graft, a kind of replacement blood vessel, but I had to fill in a lot of details on how.”
Now Laura is a Ph.D. candidate and continues her work developing the vascular graft as a graduate research assistant in biomedical engineering at SD Mines. Her research focuses on creating new blood vessels in a lab that can be used during cardiovascular surgeries to replace damaged tissues. Even more impressive, these grafts will be made out of the biological material that’s already in the human body.
Laura’s research centers around engineering substances found naturally in the human body to create new blood vessels for patients. Currently, the options for blood vessel grafting are limited to harvesting existing blood vessels from other parts of the body or using synthetic materials to create sections of blood vessels. Both of these methods have their drawbacks.
Revolutionizing Cardiology
“Our goal for this graft is to have it made out of natural polymers — materials that you would find in the body,” she explained. “A lot of grafts are made from synthetic polymers, and there’s been some success with that, but there are also downsides.”
One example of these drawbacks is with pediatric patients. A child who receives a synthetic graft will need repeated surgeries as they grow to replace the artificial vessel with a better fitting one. That won’t happen with the natural polymers being used by Laura. “It was important to me to use a material capable of being remodeled by the body, which you can do with natural polymers. The cells can actually break down those materials on a micro-level, restructure things and relay proteins as well. That allows the material to be incorporated into the tissue.”
While these grafts have the potential to be used throughout the body, Laura was particularly interested in creating a graft that can be used in the heart — replacements for coronary arteries, to be specific. Heart disease has had a significant impact on her and her family. Her father struggles with high blood pressure, and both of her maternal grandparents as well as her mother passed away from heart attacks. “Heart disease has affected everyone in my family, and it’s something that I’m very conscious of,” she said. “Our goal is to make a blood vessel, and we have the perspective of how that will make a difference in the fight against cardiovascular disease.”
The challenge with creating a replacement vessel that will be used in the heart is the amount of pressure involved. The heart beats between 60 to 100 times every minute, moving five to six liters of blood in the process. Many natural polymers don’t have the strength to withstand the constant and consistent pressure generated by the heart.
In September 2021, Laura was awarded a National Science Foundation Graduate Research Fellowship to fund her research and to provide her with a stipend while she finishes her Ph.D. The fellowship aims to strengthen and ensure the quality and longevity of the scientific and engineering workforce in the U.S., with an emphasis on diversity and broadening the participation of underrepresented groups.
Since 1952, the National Science Foundation has funded over 60,000 Graduate Research Fellowships, with more than 450 fellows joining the National Academy of Sciences and 42 fellows going on to become Nobel laureates.
A Real World Understanding
To better understand the forces that her grafts would need to endure, and to learn about how these materials might be used in the clinical environment, Laura worked with Cardiologist Bhaskar Purushottam, M.D., FACC, FSCAI, FSVMB, and Cardiothoracic and Vascular Surgeon Kalyan Vunnamadala, M.D. These physicians invited Laura to observe related surgical procedures in order for her to have a better understanding of what these grafts will need to withstand in the human body.
“They’re both really great doctors and great people. I’ve worked with Dr. Purushottam longer because he does more of the interventional work putting stents in place,” said Laura. “I shadowed Dr. Vunnamadala and got to watch him perform open heart surgery and harvest veins from the leg. Both of them have been very open to any questions and conversations with me. They communicate really well, and even though I know they’re incredibly busy, they’re also very responsive. They have been really incredible collaborators for me.”
“Synthetic polymers have their downsides, but natural polymers come with challenges as well. We can do different types of testing in the lab to understand the mechanical strength, but natural polymers and the way that they’ve been processed previously, are just inherently weaker unless we go in and modify certain things. When you make certain modifications, sometimes you can take away that ability to have the material remodeled by the body.
Our focus is really using certain polymer processing methods to take advantage of alignment of microfibers to enhance the mechanical properties of the graft. Right now, I’m looking at three, possibly four distinctively different layers. I’ve made a three layer graft out of collagen — collagen is really easy to work with just to test some of our processing methods — and now I’m back on the computer researching, trying to figure out different ways that people have processed other materials and what methods we need to use to make it more mechanically sound. Once those projects are done, I’m hoping to have most of my focus on this material’s processing to create the second generation of this graft.” Laura said.
Where No One Has Gone Before
Building a blood vessel is no easy task. It involves creating specialized equipment to even get started. Laura and her team made an in vitro modeling device that allows them to model parts of the human anatomy outside of the body. “What we’re trying to do is model this small piece of the vascular system. I can put cells in this device to simulate the endothelium, the inner lining of blood vessels, and I can do all kinds of different tests on them,” she explained.
With two years left in her Ph.D. program, Laura is focused on completing her research. “Most of my focus has been the in vitro modeling device that we built and developing the second generation of the grafts. Once we wrap those things up, I’ll probably spend more time trying to figure out what my next steps will be,” she said. “I haven’t spent a lot of time thinking about my life after school because just trying to finish the design and get the work done is consuming in itself.”
Recovering from A brain tumor AND radiation, Grayson Chapeau can once again enjoy ping pong, dancing – and life.
In October 2014, Grayson Chapeau of Spearfish was diagnosed with an astrocytoma, a malignant tumor of the brain. He was just 4 years old. It took several doctor visits to get the right diagnosis. Kids with brain tumors usually experience severe headaches, but Grayson never had that complaint.
His mom, Chelsey Chapeau, said she came to realize that Grayson has an amazing pain threshold. Also, he just doesn’t complain – about anything.
“Grayson has taught us a lot about resilience,” Chelsey said. One day, when she picked him up at school Grayson was in a particularly good mood. She asked him if something good happened at school. No, he said, “I just picked joy.”
In the past eight years, Grayson has faced more challenges than any 12-year-old should ever have to deal with. With the help of hyperbaric oxygen therapy he’s been able to move beyond those challenges.

Grayson Chapeau has recruited his classmates from Creekside Elementary and others to help him collect pop tabs for the Ronald McDonald House, a charity that provides a free place to stay for families of kids who are receiving medical treatment away from home.
Hyperbaric Oxygen Therapy
After his cancer diagnosis, Grayson underwent chemotherapy and radiation treatments under the care of pediatric oncologist Jean Mulcahy Levy, M.D., at Children’s Hospital Colorado. The treatments were administered at the Cancer Care Institute in Rapid City by nationally recognized radiation oncologist Daniel Petereit, M.D. Although the radiation significantly reduced Grayson’s tumor, his health continued to decline. He had double vision, difficulty with balance, frequent falls and painful headaches. Dr. Mulcahy and her team thought this might be due to inadvertent brain injury—radionecrosis—a side effect that sometimes occurs with radiation treatment for cancer.
He was referred to the Hyperbaric Medicine Treatment Center at Monument Health Rapid City Hospital for hyperbaric oxygen therapy. It’s a treatment that involves patients spending time in a high-pressure chamber filled with pure oxygen to saturate the patient’s circulatory system with tissue-healing oxygen.
Patrick Tibbles, M.D., is the Medical Director of Hyperbaric Medicine at Monument Health. He evaluated Grayson and felt the boy was a good candidate for this life-saving intervention.
“There are several clinical studies that show that this treatment works in a small number of pediatric patients,” said Dr. Tibbles. “It not only saves lives but produces dramatic improvement in neurologic function and clinical symptoms such as headaches.”
Over the course of several months, Grayson was placed five days a week in a hyperbaric oxygen therapy chamber and administered high concentrations of oxygen under pressure for several hours to heal the radiation-injured brain tissue. Toward the end of his treatment regimen, Grayson was able to give high-fives to his doctors, play ping pong with his brother and walk without difficulty. He also experienced fewer headaches.

Grayson works regularly with and Occupational Therapist Megan Stephens, left, and Physical Therapist Elizabeth Howorth at Monument Health Rehabilitation in Spearfifish. “Grayson’s the best,” said Elizabeth. “He puts a smile on our face every time.”
Continuing Therapy
In addition to his hyperbaric treatments, Grayson works twice a week with Physical Therapist Elizabeth Howorth and Occupational Therapist Megan Stephens at Monument Health Rehabilitation in Spearfish. Elizabeth helps Grayson improve his mobility through activities such as bicycling, jumping and dancing. Megan helps Grayson improve the fine motor skills in his right arm. When he started these therapy sessions, Grayson couldn’t even get up off the floor by himself. With each session, his motor skills have improved, Elisabeth said. “Grayson’s the best. He puts a smile on our face every time,” she added.
Pop Tab Challenge
A fifth-grader currently attending Creekside Elementary School in Spearfish, Grayson is well-known at school, where he gives free hugs to teachers. He’s also a favorite among the doctors and caregivers in the Hyperbaric Medicine Treatment Center.
Grayson also persuades other kids to help him raise money for the Ronald McDonald House through a Pop Tab Challenge. He enlists his schoolmates to collect the tabs on the tops of aluminum beverage cans.
Earlier in his medical journey, he traveled to Minnesota to see specialists. That’s where he learned about Ronald McDonald House. Even though the family has never stayed at one, Grayson was inspired by the idea of having a place where families of extremely sick children could stay.
In his first Pop Tab Challenge, Grayson collected 88 pounds of tabs. In the second year, 433 pounds. For his third year, he set a goal of 500 pounds – and collected 867 pounds. This spring, he had 1,700 pounds, well on his way to this year’s one-ton goal.

HBOT: flooding the body with restorative oxygen
Hyperbaric oxygen therapy, sometimes called HBOT, is a type of therapy in which patients breathe 100 percent oxygen at pressures two to three times the normal atmospheric pressure at sea level. Oxygen enters the body through the lungs. It’s picked up by the hemoglobin and delivered throughout the body. The process elevates oxygen levels in blood plasma, stimulates new blood vessel growth, fights bacteria, reduces tissue swelling and dissolves pathologic gas in the brain, heart and muscles. Hyperbaric therapy is a well-established treatment for radiation-injured tissue in various parts of the body including the intestines, bladder, jaw and other soft tissue areas, such as breast and the abdomen. It’s also used to treat patients whose diabetes has damaged blood vessels and ulcers in their extremities that won’t heal. It can also treat carbon monoxide poisoning and decompression sickness.
Monument Health Rapid City Hospital has two hyperbaric chambers. Patrick Tibbles, M.D., Medical Director of Hyperbaric Medicine at Monument Health, said the only discomfort patients feel is the pressure on ears, similar to diving or swimming. Once they learn to equalize the pressure and clear the ears, the discomfort goes away.
Make Today Great
Grayson once asked his mom why people are always telling each other to “have a great day.” To Grayson, the phrase implies we can’t control the kind of day we’ll have. So he changed it to “Make today great.” The family made the saying into a T-shirt for Grayson to wear. Chelsey is amazed by Grayson’s poise and maturity when he interacts with others. “He takes the time to engage with everyone he meets, and he makes them feel like a million bucks, she said. “He’s wise beyond his years.”
David and Darlene Fickbohm have embarked on a journey together. Not to a destination, but rather to a healthier life. Both are Monument Health caregivers: Darlene is a Registered Nurse who works in Utilization Review at Rapid City Hospital, and her husband David works at Sturgis Hospital as a Maintenance Mechanic. And both are patients of General Surgeon Andrew VanOsdol, M.D, at Monument Health Bariatrics and Weight Management in Spearfish.
If you mention bariatrics, many people think about weight loss surgery. That’s only part of the story, though. When you look deeper, you’ll find that the goal of bariatrics isn’t simply to lose weight, but rather to develop a healthier lifestyle. Darlene and David know this from firsthand experience.
“A lot of people don’t understand the psychological side of eating and this process, but it’s hard on you when you change from eating one way to another. Like on Thanksgiving when everyone is enjoying a lot of stuff, or when you socialize at restaurants and you’re sitting there and not partaking in the same way as the people around you. There’s a big psychological factor there, so having that education from mental health professionals is great, and you can always go back for more sessions if you’re struggling. It’s also important to have that support from others as well, because you can’t do it alone. Darlene and I did this together, which I think has been one reason things have gone so well — we’re our own support group. But there are actual support groups for people who go through this process too,” David said.
Starting a journey
Darlene initially met with Dr. VanOsdol and the Bariatrics and Weight Management team in June 2020 to discuss problems with her gastrointestinal tract. She brought with her a long list of health issues including diabetes, but even prior to her appointment she was taking steps to improve her health. A few months prior to her initial appointment with Dr. VanOsdol, Darlene and David had transitioned to a vegan diet to help with her diabetes and digestion problems, and experienced some success with it. “I lost 30 pounds going vegan, and I already felt better,” says Darlene. “But I was still having some GI issues that I really wanted to resolve.”
This began the journey to a healthier lifestyle that Darlene and David would take together, but she hadn’t expected surgery to be part of that journey. The Fickbohms were no strangers to bariatric surgery — about a decade prior, David had a lap band and nissen fundoplication procedure for gastric reflux at another health care facility. He was never fully satisfied with the results, so it’s no surprise that Darlene didn’t necessarily plan on including bariatric surgery on her health journey. Dr. VanOsdol, however, felt that she would be a good candidate for a gastric sleeve.
“During a sleeve gastrectomy, we remove part of the patient’s stomach, creating a new smaller, sleeve-like stomach in the process. Digestion works exactly as it did before, but there are changes in horemones resulting in feeling less hungry and more satisfaction after eating less food,” explains Dr. VanOsdol. “I’m always cautious about recommending surgery, but Darlene was a good candidate because of the hard work she and David were already doing to improve their lifestyle.”
“There’s a misconception that weight loss means just eating less and exercising more. There’s more going on as far as metabolic rate and even your own body working against you. Surgery isn’t an easy way out; it requires a significant lifestyle change. The goal isn’t simply to lose weight; the goal is health, so we work on a weight management program that meets all the patient’s needs. That includes the emotional component. Most people know about emotional eating, but research has found links between trauma and obesity. Not everyone struggling with obesity has experienced trauma, but it shows the effect emotions can have on nutrition.”
Slow and steady
When she decided that she would get the gastric sleeve, Darlene learned that it would be six months to a year before the procedure would occur. “I had to see a nutritionist, I had to be evaluated by a mental health professional and I needed to see Dr. VanOsdol for so long and a certain number of times to get approved by insurance,” she says. “It’s a long process, not a quick fix.”
Darlene began showing signs of success after receiving her gastric sleeve, so her husband David decided to get one as well. Like Darlene, he was a good candidate for the procedure — they had made their diet and lifestyle changes as a family, so Dr. VanOsdol felt confident that he would be successful with it as well. After removing his lap band and nissen, Dr. VanOsdol performed the sleeve gastrectomy on David as well. Together, the Fickbohms have continued to lose weight and improve their overall health and lifestyle.
Often people think of bariatrics as just a surgery — and while for many patients a surgical procedure can be incredibly helpful, it’s never just a surgery. There are several caregivers involved with a successful bariatrics program, and they all contribute different skills and experience. “Lots of people tell us, ‘I know enough about nutrition, I just need to eat less,’ but
it isn’t just how much you eat, but also what nutrients you’re getting,” said Dr. VanOsdol. “When there’s any kind of deficiency in our nutrition, that’s when we start craving things and it becomes much harder to control.”
Monument Health Spearfish Hospital, home to the Bariatrics and Weight Management program, was recently designated a MBSAQIP Accredited Comprehensive Center by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, a national organization. MBSAQIP is a joint program of the American College of Surgeons (ACS) and the American Society for Metabolic and Bariatric Surgery (ASMBS). It affirms that the hospital’s bariatric patients receive multidisciplinary medical care, which improves patient outcomes and long-term success. In addition, accredited centers offer preoperative and postoperative care designed specifically for patients with obesity. Dr. VanOsdol says that this provides the program with additional resources within the ASMBS, and that programs that are accredited have better outcomes than programs that are not accredited. The accreditation process took several years, as all accredited centers are required to treat so many cases each year, as well as to meet specific follow-up requirements. Bariatric surgery is not just about the procedure: it’s also the patient care before and after the surgery.
Dr. VanOsdol adds, “Really, that’s something that our program does really well. Providing support outside of just the surgical part of the process, from nutrition to support groups. So in many ways, the accreditation process is making sure that we’re providing education for our nurses and that we are taking care of the whole patient rather than just operating. That has always been our approach, so this accreditation is a tribute to the hard work of the surgical staff and recognition of the great outcomes we’ve been able to achieve.”
Changing perspectives
Patients work with the entire team before a procedure is scheduled. Without these building blocks, any kind of bariatric surgery is unlikely to succeed. “It builds a mindset that changes your eating habits and lifestyle. It’s not just thinking, ‘Oh I’m going to lose the weight and I’ll be done.’ I think that’s where people run into trouble,” says Darlene. “It’s an entire lifestyle change — it’s not losing the weight or getting to the size you want and then just going back to what you were doing before. Because you’ll end up right back where you were.”
“It’s not something that you can do without support,” adds David. “I think a big part of why we’ve been successful is that we’ve done this together. We’re a team, and we’ve improved our lifestyle together.” As a family the Fickbohms continue to lead a healthy lifestyle. They’ve each lost about 100 pounds, and their son has come along on the journey as well, losing over 100 pounds through diet and exercise. Darlene no longer has to take medication for her diabetes, and has reduced the amount of medication she has to take for blood pressure. Most importantly, the entire family feels healthier and has more energy.
“That’s what it’s all about,” says Darlene. “Not just weight loss, but having a healthier, and more enjoyable lifestyle.”
Many people struggle to lose weight and keep it off. That’s why Monument Health caregivers approach weight loss with a whole-person approach.
Kennedi Springstun had what most would consider a normal pregnancy. Other than the typical discomforts of pregnancy, the mother-to-be felt healthy and excited to meet her baby, Linkin.
On July 31, 2021, three weeks before her due date, Kennedi began having contractions. Concerned, she and her fiance, Derek, headed to Monument Health Spearfish Hospital. When they arrived, Kennedi was already 4 cm dilated and entering the active phase of labor. Her concern turned to worry as the nurses began to prep her for delivery — at just 36 weeks and 6 days, she feared it might be too early.
The delivery began with no issues. Kennedi was given an epidural and began pushing normally. Everything went according to plan until the baby was delivered. Linkin was limp, blue and wasn’t breathing. The delivery team immediately brought him to Dr. Bigwood, who was unable to locate a heartbeat and began resuscitation at once. Because Linkin didn’t respond immediately, he was brought to the nursery where resuscitation continued. Dr. Bigwood suspected that the newborn had a congenital diaphragmatic hernia (CDH).
CDH is a birth defect in which the diaphragm — the muscle that separates the abdomen from the chest — doesn’t develop completely, resulting in a hole that allows the abdominal organs to migrate into the chest. When that happens, the lungs don’t have enough space to develop normally, making it difficult for the baby to breathe, while also crowding the heart. X-rays soon confirmed the pediatrician’s initial assessment, and in Linkin’s case, the heart was so crowded it had been pushed to the opposite side of his chest.
Jonathan Bigwood, M.D. is a pediatrician at the Monument Health Spearfish Clinic – North Avenue. The family has always been a central point of focus, and he recognizes the essential contribution families make towards children’s happiness and well-being.
Born in the City of London, at eight he moved with his parents and six siblings to the countryside. Growing up on a small farm, he learned a great deal about nature, how to care for animals and the value of working hard. He gravitated towards sciences in school and loved to read and learn new things. Those experiences helped steer him towards a career in medicine.
Spending time together is very important to Dr. Bigwood’s family. His wife and daughter enjoy discovering new things in their surroundings and feel very fortunate to be here.
One of the common experiences among parents is the anticipation of hearing their baby’s first cries. It’s an infant’s first interaction with the world around them and a signal to moms and dads that everything is okay. Kennedi didn’t hear that cry when her baby was born, or even see him.
But Kennedi and Derek put their trust in Dr. Bigwood, and more than 20 years of pediatric experience in three major children’s hospitals across the country gave him the insight necessary to diagnose the condition immediately. While the OB/GYN team cared for Kennedi, Linkin was intubated and stabilized for transport. After being taken to Rapid City by ambulance he was airlifted to Sioux Falls.
“It was the worst and best day of my life,” Kennedi reflects, shaking her head.
“This is a serious condition,” notes Dr. Bigwood. “It is very difficult for these kids to breathe, and it is not a condition that is easy to survive. These babies have to go from the delivery room to surgery straight away.”
It took nearly two days to stabilize Linkin to the point he was strong enough to undergo surgery to repair the hole in his diaphragm. He spent 27 days in the Neonatal Intensive Care Unit (NICU) in Sioux Falls following the procedure. Kennedi remembers driving to Sioux Falls to meet her son for the first time, “It was like going on a first date. I was so nervous.”
The Monument Health Neonatal Transport Team consists of registered nurses, neonatal nurse practitioners and respiratory therapists specially trained in the stabilization, management and transport of ill and premature newborns by ambulance or airplane. The transport team is available 24 hours a day, 7 days a week.
The doctors assured Kennedi and Derek that it had been a great outcome, although at times it was difficult to stay positive. For the first three weeks of his life, they couldn’t hold their son, who was on a ventilator and feeding tube. “I would feel sick every time I would go up to the NICU,” Derek says, remembering the emotional toll it took on him. “Hearing the babies crying was so hard.”
As is the case with many things, challenges lead to greater rewards — or in this particular case, struggles give way to snuggles. Linkin’s parents dote on him, and the days of not being able to hold him are long gone. Their hugs and kisses are plentiful, as are the smiles he gives back. Linkin has no long-term damage from CDH. He has completely recovered, and is a healthy infant. As Dr. Bigwood says, “He’s good! Look at him! Had you not known the whole story, you would never know there was anything wrong.”
Linkin is pretty fond of Dr. Bigwood, who will be his pediatrician for the foreseeable future. He’s not the only one who appreciates the physician: “He saved his life,” Kennedi says of the pediatrician as she smiles at Linkin.
There’s plenty of gratitude to go around: Kennedi and Derek are grateful for Dr. Bigwood; Dr. Bigwood is grateful for his training and experience which made it possible to recognize Linkin’s condition so quickly; all are grateful for the incredible caregivers and physicians that were part of Linkin’s care team. “We are a small hospital, but we are not small in what we handle,” Dr. Bigwood reflects. “I have worked at some of the biggest children’s hospitals in the country and we handle what they handle. Our team is just as dedicated.”
Pediatricians throughout Monument Health offer preventive care services such as well-child visits and immunizations, as well as care for a wide range of illnesses and chronic health conditions.
Leah Nixon has an edgy sense of humor, which comes in handy when writing and designing a line of greeting cards. But humor was an absolute necessity during her long, painful recovery from an accident that left her paralyzed below the armpits and required doctors amputate one of her legs.
An example of Leah’s humor: while describing how she felt about being transferred to Craig Hospital in Denver, one of the world’s best spinal cord injury rehabilitation centers, Leah said, “It sounded so magical to go from being a slug in a bed to, like, being able to do laundry and drive again.”
Did she really feel like a slug in a bed?
“Actually, I told my family I felt like a rotisserie chicken on a bed of ice,” she deadpans.
A year before her accident, Leah and her sister, Grace Nixon Peterson, became partners in Tiny and Snail, a company that designs and prints greeting cards, postcards, stickers and other products. Grace had started the company, at the time selling hand-painted cards. The work was hard on her wrists, so Leah began helping out.
“I told her ‘I think we should go into business together. I can be your hands, and you can be my brain,’” Leah recalled.
The sisters, 32 months apart in age, were already close. But collaborating on cards and running the business brought them even closer together, even though Leah lives in Rapid City and Grace lives in Milwaukee.
The Accident
In 2018, Tiny and Snail wasn’t paying the bills, so Leah kept her day job working construction in Rapid City. On August 14, 2018, a forklift tipped over at a job site, crushing her and severing her spine.
Grace remembers the terrible phone call from her mother about the accident. “I remember wailing on the couch that night with my husband, and he just held me and I said, ‘God, you have to let her live and you have to let her still use her hands.’ It was definitely the worst day of all of our lives, and it was difficult flying to see Leah, just hanging by an absolute thread.”
Leah was in the intensive care unit at Rapid City Hospital for 29 days. With a breathing tube in her throat and under anesthetic, Leah was unable to speak. She communicated by tracing letters on Grace’s palm.
Her first question: “Can I still draw?”
Grace Nixon Peterson and Leah Nixon have built Tiny and Snail into a successful business, marketing directly to customers online at tinyandsnail.com. Their Instagram account, @tiny_and_snail, has been well received.
Both Leah and Grace draw the images and write the text for their products. Sometimes they collaborate. Sometimes they work separately. However all of their cards, stamps, stickers and other designs share the same smart, simply worded and brightly illustrated style.
More recently, Grace and Leah have been focusing on the wholesale side of their business, selling through retailers and gift shops.
Gifts With Heart, the gift shop in the lobby at Monument Health Rapid City Hospital, is a Tiny and Snail outlet.
ICU Dance Party
Leah later graduated to writing on paper with a Sharpie. She started telling jokes to put the family at ease. “It was really funny because we’re just kind of waiting on pins and needles, and then I say something totally unexpected and the tension just goes away.” Leah recalled.
Grace added, “It was like the joy was amplified because the pain was amplified.”
Even though Leah was very weak, the neurosurgeon urged her to keep using her arms at least once every hour to stop the paralysis from advancing.
“My family was kind of militant about it, but I said, ‘This would be a lot easier if we turn on some music.’ So then we started having dance parties in the ICU. The nurses would join in sometimes,” Leah said.
After recovering enough to travel, Leah was flown to Craig Hospital in Denver where she began her long recovery and extensive rehabilitation.
Life Today
Leah lives in Rapid City with her husband, Kelsey Fitzgerald, and her dogs, Lucy and Ryder. In June of 2021, Leah gave birth to a baby girl named Ellie Grace Nixon Fitzgerald.
Family remains very important to Leah. She lives a couple miles from her parents and talks often with her siblings. Every year on August 14, the whole family gathers to celebrate — not mourn — the anniversary of Leah’s accident. “From the get-go, we decided to reclaim that day and make it a celebration,” Grace said. “We call it ‘Leah Lived Day.’”
Despite her strength, humor and family ties, Leah said it’s hard to accept she still lives every day in extreme pain. People assume if someone is paralyzed they have no feeling. The reality, at least for Leah, is that she spends every waking moment feeling like she’s receiving electric shock or sitting in ice water.
“When I go to the doctor, they always ask me to describe my pain on a scale of 1 to 10… You would need letters to describe my pain; you can’t put it on a scale of 1 to 10,” she said.
In spite of her pain, Leah and Grace feel the accident has transformed their art and their lives. Leah loved art before, but wasn’t sure what she wanted to do with her life. The accident let her truly focus on what she loves.
Grace believes Leah’s accident brought new depth and compassion to their creations at Tiny and Snail.
“There’s something about being thrown into this crazy life situation and traveling to the depths of tragedy,” she said. “I think it’s just given us such an empathy for being human and enduring the hard things that can happen. That’s helped us create art that gives others the words to support each other.”
In addition to Tiny & Snail’s greeting cards, Leah recently illustrated a children’s book.
“Best Day Ever” was written by award-winning author Marilyn Singer. It’s about a boy’s adventures with his energetic dog, and how they go from a bad day to making it the best day ever.
The young boy happens to be in a wheelchair, and the book’s publisher wanted an artist in a wheelchair to illustrate it. Leah thinks it was the perfect story to be her first book.
Mention Brady Thompson to pretty much anyone in Buffalo, and they’ll respond with a smile. Everybody knows this pint-sized 7-year-old, and they agree he’s a character.
Brady lives on the family ranch southwest of town with his parents, two older sisters, a dog, a cat and three goats. He’s outgoing, talkative and has a fondness for spicy food – the hotter the better. He can talk ranching like an old timer, but when asked to pose for a photo inside the goat pen, Brady firmly replied, “Ah, no.”
“He has kind of an old soul,” said his mom, Terisa Thompson. “His teacher told me he thinks the other kindergartners are too noisy. He’d rather sit down over a cup of coffee and talk about life.”
“He’s so cute. He carries hot sauce everywhere,” said Crystal Page, the physician assistant at Monument Health Buffalo Clinic. She has cared for Brady for much of his young life.
It’s a childhood that almost didn’t get this far. Brady was born with hypoplastic left heart syndrome, a rare condition in which the left ventricle is underdeveloped. Before he was 3, Brady had undergone open heart surgery three times, the first when he was just two days old.
Not long after returning home from the third surgery, Brady started crying and grabbing at his chest one afternoon. The family called 911. His dad, Mac Thompson, scooped the child up and they headed for help. By the time they made the bumpy 7-mile drive to the nearest paved road, Brady was completely limp.
When they reached the highway, Crystal Page, PA-C, and Jennie Glines, RN, of the Buffalo Clinic were there to meet them. They stabilized Brady’s condition and made sure he was ready for the 80-mile ambulance ride to the hospital in Spearfish.
It means that the left side of his heart didn’t fully develop before birth. The right side pumps blood to the lungs, but the left side can’t properly pump that oxygen-rich blood to the rest of the body.
Brady pulled through, but still needs regular medical care. Along with a list of other medications, he takes blood thinners that require regular blood tests.
At one point early in his illness, Brady’s parents seriously wondered whether the Thompson family could stay on the Harding County ranch that has been in Mac’s family for more than 100 years. Fortunately, the three-person staff at Monument Health Buffalo Clinic provides a surprising breadth of medical services for Brady and his neighbors throughout the Buffalo area.
Wide Open Spaces
Harding County, in the far northwestern corner of South Dakota, is about as rural as you can get. With 0.47 people per square mile, it’s South Dakota’s least-densely populated county, and the 24th least-densely populated in the United States. But the rolling prairies, sweeping views and quiet serenity offer an attractive lifestyle for Harding County’s 1,200 residents.
Buffalo — population 350 — has a selfsupporting downtown business district. There’s a SuperValu grocery store on Main Street, a few doors down from Buffalo Hardware and Lumber. Buffalo also has convenience stores, a handful of bars and restaurants, a modern school that hosts grades K–12, a bank, a couple of churches and a post office. Tucked away on Ramsland Street a block north of Main Street is the Monument Health Buffalo Clinic.
Staff at the Monument Health Buffalo Clinic consists of Crystal, a physician assistant, Jennie, a registered nurse, and patient access specialist Ann Parfrey. Ann is also an emergency medical technician, which allows her to assist with checking patient vitals and other clinical duties.
Part of the Community
On a recent Thursday afternoon, the clinic waiting room had a handful of patients, including Steve Pemble, who was stopping in for his COVID-19 vaccination. Steve joked with Ann before heading back to get his shot. The COVID-19 vaccination is a good example of the importance of having health care close to home. Spearfish is a three-hour round trip; a long drive for a shot that takes fewer than 20 minutes.
It helps that Crystal, Jennie and Ann are woven into the fabric of the Buffalo community. Crystal grew up in Nebraska, and Jennie is from Spearfish — but they are married to Harding County natives. Crystal has four school-age children who attend Harding County School. Jennie’s two kids are not old enough for school yet. Ann’s three grown children completed school here.
Crystal, Jennie and Ann know the families, attend school events, go to football games – occasionally opening the clinic on a Friday night to X-ray a football injury. They are active in the community and well-known.
It's one of the lowest population densities of all counties in America. By comparison, the Island of Manhattan has almost 70,000 people per square mile.
Meeting the Needs
The Buffalo Clinic is fairly well-equipped. Monument Health recently installed a new X-ray machine, and the lab has an Abbot ID Now analyzer for diagnosing COVID-19. They can also process several lab tests inhouse, including analysis of blood samples for heart patients like Brady. Tests that can’t be processed in-house are sent to Rapid City Hospital, usually with a one-day turnaround.
“We have to be well-equipped,” said Crystal. “Otherwise, what’s the point of having a clinic?”
The team works closely with the ambulance service. In fact, there are times when they’ve had to close the clinic so Ann, Jennie and Crystal could respond to a serious automobile accident. “When things like that happen, patients with appointments are gracious about rescheduling,” Crystal said.
Favorite Patient
When Brady Thompson stops by the clinic, hot sauce in hand, he brightens everyone’s day, Crystal said. On a recent visit, Jennie told him that Cheetos has a new Cheesy Jalape o Mac ‘n Cheese. His eyes grew wide, and he turned to his mom and said, “We need to get that!”
Apparently a fondness for spicy foods is not unusual for youngsters with hypoplastic left heart syndrome, according to Terisa.
How else can you explain that a 7-yearold’s favorite snack is bread dipped in Tabasco sauce?
In addition to the rural clinics in Belle Fourche, Hill City, Hot Springs and Wall, Monument Health also runs critical care hospitals in Custer, Deadwood and Sturgis.
Coming to Monument Health may sometimes mean patients and their families are experiencing some of life’s biggest hardships. With this in mind, the team at Monument Health wanted entering the doors on Fifth Street to feel like walking into somewhere familiar. The stone facade evokes our golden South Dakota prairies; while inside visitors are greeted by pictures of Spearfish Canyon, Custer State Park, the Badlands and more. In a word: home. Whatever brings patients to Monument Health, creating familiarity helps take the stress off their shoulders as they are embraced by the world-class, caring staff.
Marcia Taylor, RN, has worked for Monument Health for 46 years; a journey she says has been gratifying due to her variety of job experiences. But even more importantly, Monument Health has been there for her and generations of her family in some of their toughest times.
Her mother-in-law, now 93, was hospitalized years ago for a broken hip. Amidst a tough situation, Marcia says “Monument Health really stepped up and helped her recover, with great outcomes, and now she’s in good health.”
Marcia’s husband, Randy Taylor, has also spent time in the care of Monument Health. A number of years ago, Randy called Marcia to tell her his back hurt. “I told him to come in, and on the way in he blacked out and his truck left the road” Marcia says. Both Randy and their son were transported to the Emergency Department and treated upon arrival. Their son was fine, and while Randy had suffered a heart attack, he recovered well under the care of Monument Health.
No matter what her family has had to visit Monument Health for—when Marcia gave birth to their sons, various trips to the Emergency Department that come with childhood, even Randy’s open heart surgery—Marcia says that their entire family is grateful for the specialties and level of care that Monument Health provides. Not only that, she says “everyone at Monument Health really focuses on their patients. It’s not just about the medical outcomes, they make sure that your care serves you and your goals.”
Patients and Families
Marcia Taylor RN, is a Clinical Coach at Monument Health. It’s a role that allows her to give guidance in clinical situations and work with patients, families and staff to find the best plan of care. “We know that environment can create healing effects,” she explains. “A lot of work went into talking about what healing means and how that can be shown through physical structure.”
This resulted in not only reworking the Fifth Street Entrance at Rapid City Hospital, but also the healing room, garden, and other quiet places where people can take a moment and refocus. “The majority of people in acute care settings did not plan to be there,” Marcia says. “Their whole life is disrupted, causing significant stress. Quiet areas allow for a moment of reflection or prayer, or even just being with loved ones in silence for a little bit.”
It’s also about the family; health care settings help foster a connection between generations. Children might be visiting parents or grandparents, and everybody is feeling stress over the experience. “You just strive to see what you can do to meet their needs with the situation at hand and make their experience as individualized as possible,” she says. “We like their feedback and want to make sure it improves their outcome. That’s our goal and something we should be doing every day.”
This brings a human element to what is often a difficult and unsettling period in an individual’s life, and is at the heart of patient-centered design, a concept that puts an emphasis on quality care and patient satisfaction.
Comforting Yet Functional
While the new entrance is aesthetically appealing, the goal for this construction project wasn’t merely cosmetic improvements. With the busiest Emergency Department in the state of South Dakota, the need for more space—and more efficient use of that space—was the overriding impetus for the expansion.
John Pierce, President of Rapid City Hospital and Market, has dreamed of expansion ever since joining Monument Health 21 years ago. He was particularly passionate about bringing heart and vascular care onto the Rapid City Hospital campus.
"We are an important asset to our community, so being able to grow our campus in a way that will help us better serve our communities for years to come is very exciting,” John says.
The addition of 380,000 square feet of building space includes a brand new Emergency Department; complete with rooftop helipad and a drive-through ambulance garage. There’s also the newly relocated Heart and Vascular Institute, and the Heart and Vascular Unit which combines a 32 private room inpatient facility with outpatient cardiovascular services all under one roof.
Art as Healing
When selecting artwork, Monument Health’s curation team focused on how each piece would impact both patients and caregivers. Choosing art that creates a sense of familiarity and calm has been proven to relieve anxiety associated with a health care environment and ultimately decrease stay times. Not to mention, the presence of art reduces stress and increases satisfaction for caregivers, enabling them to better assist those trusted to their care.
While spending money on art may seem strange in a health care setting, Monument Health believes that health care needs to be functional, not institutionalized. Patients have enough stress when they walk in the doors, the space they walk into should be welcoming and comforting. The new art installation does exactly that, welcomes patients in, make them feel at ease, assists in their healing and helps them continue their life’s journey.
Monument Health used a patient-centric model that focuses on reducing patients’ stress and anxiety, which increases positive outcomes and reduces hospital stay times.
Farm to Fork
The farm to fork movement (also known as farm to table) got its unofficial start in the 1960s during the countercultural revolution, when hippies began growing their own food locally and organically. Renowned chefs like Alice Waters, whose influential restaurant Chez Panisse opened in 1971, embraced the concept of local, sustainable agriculture, helping to push the movement into the mainstream. Today, it’s not uncommon to find restaurants in South Dakota and across the country marketing farm to fork dining, as processed foods fall out of favor and Americans adopt healthier lifestyles.
Put simply, farm to fork is a food system in which food production, processing, distribution, and consumption are integrated to enhance the environmental, economic, social and nutritional health of a particular place.
It consists of four principles: food security, proximity, self-reliance, and sustainability. The basic idea is that communities should have easy access to locally grown food, eliminating the need for outside suppliers. With farmers markets gaining in popularity and because consumers are more conscious than ever about the effects of food on their health, the farm to fork movement has seen explosive growth—especially over the past eight months, as the food chain has come under increasing scrutiny.
Food Supply Chain Disruptions
COVID-19’s impacts have been wide-ranging, and the food supply chain is no exception. We witnessed this early on when plant shutdowns across the country led to meat shortages. When restaurants began closing their doors nationwide or switching to takeout service only, the opposite problem occurred: there was too much food and not enough space in which to store it.
Consumers contributed to these supply chain disruptions through panic buying and hoarding, leading to empty shelves. While stores are better stocked these days, the problem persists because of labor shortages in the agricultural industry and shifting demand associated with on-again, off-again lockdowns and restaurant/school closures. Factor in smaller spending due to loss of income—a trend that affects nutritious foods such as fruits and vegetables more than most others, the very heart of the farm to fork movement—and it’s evident that supply chains will continue struggling to keep up with demand.
While many organizations struggled to keep meat and produce on shelves at the beginning of the COVID-19 pandemic, Monument Health wasn’t one of them. Using local food sources ensured patients and their families always had food available, so they could focus on their health.
Natural and Organic
With more of an emphasis on locally grown and sourced produce and meat, natural and organic foods are surging in popularity. Though they’re often lumped together, there are some key differences between the two.
“Natural” foods are perceived to be pure and healthy, but the United States Department of Agriculture (USDA) doesn’t regulate use of the word on product labels for crops. Natural foods might actually contain pesticides, as well as genetically engineered and highly processed ingredients. Organic foods, by contrast, are heavily regulated by both agencies. Foods that are labeled organic contain no toxic pesticides, chemicals, synthetic growth hormones, antibiotics, genetically modified organisms (GMO), artificial additives or preservatives. While organic foods are always natural and pesticide-free, consumers don’t always have to buy organic. Theresa Ferdinand, Manager of Employee Health & Wellbeing at Monument Health, says consumers should focus on meat, milk, and eggs above all else. “Those are where you’d want to spend your money,” she says.
For additional information, consult the “Dirty Dozen” (foods most likely to be contaminated by pesticides) and “Clean 15” (non-organic items that are generally safe to purchase) lists.
Michelle and Rick Grosek of Bear Butte Gardens near Sturgis say three things contribute to eating healthy: organic, local and fresh. Any one is going to lead to better nutrition, and all three together will build your health, your community and your food knowledge. We enjoy being THAT neighbor (producer) and coordinating with other producers to help build a healthy food community.
Product Traceability
Monument Health Executive Chef Scott Brinker says it’s important to know the story of your food. A lot of produce sold in western South Dakota is sourced from Florida or Mexico; it’s impossible to know the growing conditions without that traceable story. For this reason, he sources his beef and produce from local farms that allow him to investigate where his food is coming from and inspect the growing conditions firsthand. He is able to see the whole story of his food and pay attention to his carbon footprint in the process—everything from the grass the cows are eating to the soil and nutrients feeding that grass.
The Rise of Meal Kits
With COVID-19 forcing many restaurants to close and the cramped aisles of grocery stores leaving many shoppers jittery, consumers turned to meal kits as a convenient, socially distanced alternative. Meal kits take the guesswork out of cooking, providing ingredients and step-bystep instructions even the most novice of cooks can master. Best of all, they’re delivered right to the consumer’s doorstep. They’re the perfect model for sheltering-in-place and avoiding potential exposure to coronavirus.
Nutrition Confusion
Most of us at least make a halfhearted attempt to eat healthy, balanced meals, but nutrition is an area where there is ever-changing (and often conflicting) information. Knowing what to eat can be confusing! Yet, it’s crucial we get it right. Theresa says, “Nutrition is key in overall health and wellness—not only in preventing and treating chronic conditions, but being able to be at your peak and perform all day long.” While exercise is important, Theresa adds, “You can’t out-exercise a bad diet.”

The Chef
My Role
I'm the Executive Chef, responsible for all food that comes and goes within the Rapid City Hospital. Cafe Nourish is a full-service cafe with a grill, salad bar, deli station, and outdoor cooking area; create Bistro is more upscale, with a focus on vegan and vegetarian dishes. Both are open to the public.
My Goal
Instilling pride and excitement for cooking. Also teaching the next generation of cooks and chefs to understand and respect food and appreciate the important role they play in the hospital; food is medicine.
My Passion
Anything with fresh ingredients. I'm locked into wholesome, all-natural foods. It's also important to know the story of your food. I can go out to the patsture and see the cows, and the grass they're grazing.
Top Tip
Keep it simple! Don't overthink food with fancy stuff; make a recipe with 6 ingredients, execute it well, and make it look and taste good. Everything else comes with time.
Creamy Butternut Squash Soup
This hearty soup is always a big hit at Cafe Nourish. The medley of spices will warm you up-perfect for a chilly day in the hills!
Prep Time
15 min.
Cooking Time
45 min.
Yield
Serves: 10
Ingredients
- 1 pound butternut squash
- 2 cups apple juice
- 1/2 cup yellow onions, diced small
- 2 tsp Kosher salt
- 2 tbsp honey
- 1 tsp fine ground black pepper
- 1/2 tbsp ground ginger
- 1 cinnamon stick
- 6 cups boiling water
- 1/8 tsp canola oil
- 6 tsp vegetable stock
Step 1
Mist the bottom of a medium soup pot with oil. Over medium-high heat saute the onions until they become slightly translucent.
Step 2
Add the diced butternut squash and saute a little longer (2-3 minutes). Add the apple juice, water, vegetable base and honey. Bring to a boil and reduce to a simmer. Add the cinnamon stick, salt, pepper and ginger. Simmer for 45 min-1hr or until squash is fully cooked.
Step 3
Discard the cinnamon stick. Transfer the soup to a blender and puree until silky smooth. Pass the soup through a strainer, taste and adjust seasoning. Serve right away, or chill to 40 F within 4 hours. Can be garnished with pumpkin seeds, cilantro, pecans, apples, cinnamon, or crème fraîche.
Nutrition Facts Per Serving:
Calories 72.8
Carbs 17.2g
Fat 0.6g
Fat Calories 5.5
Saturated Fat 0.1g
Protein 1g
Cholesterol 0mg
Fiber 1.4g
Sodium 475 mg
Sugar 9.8g
Eating well and making smart choices isn’t all that difficult. There are several things you can do, according to Theresa. Portion control is huge; aim for moderation, and stick to fruits, vegetables, lean cuts of meat, and whole grains. Avoid sugar and refined grains as much as possible. Theresa recommends keeping a food diary or using an app, such as MyFitness Pal, to hold yourself accountable. Similarly, using an app to keep track of steps can be a good motivator to get moving.
Having trouble practicing portion control?
If you’re going out to eat, ask for a to-go box when you place your order and package up half your food before you even start eating. Whether dining at home or in a restaurant, take your time eating, and pay attention to hunger cues. Stop eating and push your plate away the moment you feel full.
A balanced diet is important, but sleep and exercise are also critical components to our health. Kari Anders, a Physical Therapist at Monument Health Lead-Deadwood Hospital, says “The effects of sleep and exercise are far-reaching, spanning across the brain and body systems. They affect cardiovascular health, immune response, energy levels, concentration and memory—just to name a few.” Luckily, we don’t need to sign up for a marathon to reap the benefits. Kari says “People who engage in even low to moderate exercise report an increase in energy levels.”
On the Rise. The number of Google searches related to bread and sourdough has shot up, reports show there’s been a 5-fold increase for the term “sourdough” since early March 2020.
My role
As Director of Anesthesia services, I serve as a leader of change and advocate of quality care. Strategic thinking and teamwork are essential components to managing anesthesia services for multiple operating rooms, endoscopy suites and a wide variety of procedural areas outside of the main OR. Our service covers Rapid City Hospital, the Orthopedic & Specialty Hospital and Same Day Surgery Center. I work in collaboration with CRNAs, anesthesiologists, surgeons, department leaders and organizational administrators to ensure OR productivity, customer satisfaction, regulatory compliance and positive patient outcomes. Along with managing day-to-day operations, I also oversee budgets.
My goal
My goal is to continue leading a team of anesthesia professionals that provide high-quality care to patients of all ages. It is important for me to support my team and help others understand the significance of our work and its impact on hospital operations. CRNAs are Board Certified Advanced Practice Providers that are specifically trained in the delivery of anesthesia. Our CRNAs are continuously at the patient’s side while they undergo their procedure. We are responsible for monitoring, putting the patient to sleep, insertion of advanced airways, titration of medications, pain management and ensuring the patient’s safe emergence from their anesthetic. Our goal is to ensure our patients are safe and remain sedated and pain-free during surgical procedures.
My passion
I am most passionate about building a team that sets the bar high in providing exceptional patient care. We strive to meet and exceed organizational goals. We work in the Anesthesia Care Team model and embrace the collegial relationship built with the anesthesiologist at West River Anesthesia. Collaboration between CRNAs and anesthesiologists in delivery of care contributes to the positive outcomes of our patients.
My role
I have been an otolaryngologist for 23 years. I am trained in the diagnosis, treatment and surgical evaluation of ear, nose, throat, head and neck disorders.
My goal
I deeply care about the overall health of my patients; my goal is to take the best care of my patients as possible. One of my goals is to increase the care of allergy and asthma patients, in conjunction with their primary providers and other specialists. I care about my patients’ overall well-being. I enjoy discussing other health concepts that may not be directly related to ENT, like vitamin D levels and improving diet and lifestyle to lead a healthy overall life.
My passion
I used to own my own farm and hayed and fixed equipment. I still enjoy being outside, whether I’m doing a landscaping project, working on my home greenhouse and garden or going hiking and hunting.
My team
I am fortunate to work alongside passionate health care professionals in Rapid City and Spearfish, who share my interests and goals for our patients. We are a dynamic team and continuing to grow with the addition of a new audiologist in Rapid City and the growing allergy practice.
For Rapid City-area real estate agent Nick Dupont, friendship with an orthopedic surgeon eventually led to a new outlook on long-persisting injuries and a trusted source of care for a loved one.
Nick was rear-ended in traffic in 2020 and has been on a journey of recovery ever since. As time went on, Nick continued to seek treatment for the ongoing effects of the wreck, but did not want to accept that “toughing it out” may be a new normal for him. He was frustrated by a lack of progress that held him back from his active lifestyle. Nick needed a second opinion, and he ended up getting one from his friend, Orthopedic Surgeon Daniel Lochmann, M.D.
The two met when Nick served as the real estate agent during Dr. Lochmann’s relocation from Wisconsin in early 2019, and the two have been friends and business associates ever since. One evening while playing golf together, Nick lamented his continuing difficulties with healing. Dr. Lochmann suggested they reconvene the discussion at Monument Health Orthopedic & Specialty Hospital, inviting his friend to see him as a patient.
“Nick is a really physical guy and is really active, but he was struggling with some things,” Dr. Lochmann said. “I told him I’d be happy to take a look.”
Nick had an MRI shortly thereafter, which led to Dr. Lochmann recommending surgery with Joseph Humpherys, D.O., FAAOS.
“Nick certainly had some deficiencies in function with his rotator cuff, and some issues with the biceps tendon as well,” Dr. Lochman said.
While in pre-op, Nick was briefed by Dr. Humpherys and also got a visit from Dr. Lochmann, who stopped in to wish his friend well.
“This is precisely why we have our team of surgeons who have multiple specialties,” Dr. Humpherys said. “Collaborating with Dr. Lochmann to help this patient is an example of our practice here.”
Nick had the procedure in late October and is eagerly awaiting the end of his 6-month recovery window to resume full activity. He and his wife, Alicen, stay busy with three children and their business.
Now that he has nearly recovered, Nick is much more optimistic about his healing and returning to his active lifestyle. “It’s made a world of difference for me. It’s given me comfort that I needed, because I was just managing before. It’s a lot better, that’s for sure.” Nick said.
“I’m looking forward to getting back into some things,” he added. “My family is, too.”
While Nick expressed his gratitude for his friend’s assistance, he may have seen more of the Orthopedic & Specialty Hospital than he wanted to this past year. Nick once again found himself in Dr. Lochmann’s care when his son, Blake, 15, had an accident at school and suffered a broken collarbone.
“Blake’s clavicle didn’t reset on its own the way we would have liked, so we ended up putting in some plates and screws to get it lined up again,” Dr. Lochmann said.
He was glad to see Blake make a full recovery, although Nick said ending up on the operating table was not an example he hoped his son would follow.
“I was joking that Blake wanted to be just like me,” Nick said. “Now we have the matching scars to prove it.”
Story and photos by Bob Slocum
“As program manager of Children’s Miracle Network (CMN) with the Monument Health Foundation, I’m responsible for raising funds that support our pediatric patients. These funds help local kids, from infants requiring critical care in the NICU to older children treated in the pediatric unit. Support for CMN plays a significant role in the comfort and care of those young patients.”
Children’s Miracle Network is a national organization that was founded more than 40 years ago to empower local communities to support health care for children. There are 170 CMN programs in the United States and Canada.
Monument Health launched its CMN program in 1989. Shawn joined the program in 2010 and took over as program manager five years later. Today, CMN raises approximately $800,000 each year through local efforts. It’s become so successful that last year Monument Health’s program was awarded a national award from CMN — the Highest Percentage Increase Award — for 138.69 percent year-over-year growth.
“This percentage was the highest of all 170 hospitals, big and small, in the entire CMN network,” said Hans Nelson, Director of the Monument Health Foundation. “This wouldn't have happened without Shawn at the helm.”
Monument Health CMN provides funds for a wide range of supplies and equipment for children being treated. That might include a $35,000 Giraffe bed for premature infants in the NICU to simple comfort items such as blankets, toys and games for children in the pediatrics unit. It could mean helping with travel expenses for a sick kid or providing helmets to youth in the helmet safety program.
The newest CMN fundraising event, launched two years ago under Shawn’s leadership, is the Golden Guitars Gala.
In partnership with Rapid City native Kory Van Sickle of the band Kory & the Fireflies, the Golden Guitars Gala brings a bit of musical glamor to the CMN mission.
Kory designed a custom guitar for Monument Health CMN, a fully-functional, ribbon-shaped gold flake model. When musical acts perform at The Monument in Rapid City, they’re asked to sign one of the guitars. Kory also uses his musical contacts to get guitars autographed by artists around the country. Then, on the second Saturday of June each year, CMN holds its Golden Guitars Gala in Rapid City, where they auction off 18 to 19 autographed guitars.
Guitars have been signed by music superstars like Willie Nelson, Morgan Wallen, Foreigner, Journey and many more.
In just two years, the event has raised more than half a million dollars. “A lot of that success is because of Shawn's leadership, attention to detail, communication and overall event execution,” said Hans.
For more information, visit monument.health/goldenguitars.
“My goal is to generate as much support for CMN and young patients as possible,” Shawn said. “This isn’t just about a dollar amount — although every cent helps kids in our community — it’s also about connecting to the community and finding ways to reach people who want to help.”
With Shawn leading the program, CMN raises funds through events and programs, including a golf tournament, mediathon, corporate partnerships and more. “Every single dollar raised in our community stays in our community,” Shawn said. “We have very strong local support, and it makes such a huge impact on the program and the kids in our care.”
While Shawn doesn’t work with patients directly, he’s passionate about the idea that his work has a direct impact on them. It makes his job especially rewarding. He also enjoys helping donors find their own passion — a cause they want to support in CMN. “Making a charitable gift can be highly personal and for many of our donors it is a well-though-out decision," he said. "We value belief in our purpose, and we want our supporters to understand the impact they have on our pediatric patients.”
“In one of my first jobs out of college, I worked at a Colorado golf resort known for exceptional customer service. I learned how to bring events to customers and create the very best experience for them. I do my best to bring that same philosophy to my work at CMN,” Shawn said. He goes out of his way to ensure that donors feel connected to the cause through flawlessly planned events like the Golden Guitars Gala and personalized experiences like meeting some of the children who have been helped by CMN funds. The relationship building in his work is what brings him particular joy.
“I get to meet and work with so many amazing people and help connect them to the cause,” he said. “It’s the best part of my job.”
Story by Lynn Taylor Rick
Photos by Bob Slocum
Like a lot of high school seniors, Morgan Geppert doesn’t have much to say about herself. “I like to work, and I like to read sometimes,” she said. “I love skiing.”
Her father, Travis, nodded his head, and added, “It’s pretty much always been her thing. She has two brothers and one sister, and they each have something that they’re passionate about. For Morgan, it has always been skiing. She was a natural, and just graceful and confident on her skis.”
Morgan is cool and calm — even a little aloof, in a fun way — despite not knowing exactly how to answer questions about herself. Sitting and talking with her, it’s unlikely that you’d have any idea that Morgan dealt with a devastating injury. In a cruel, poetic twist, she was hurt doing what she loves most — skiing.
The crash
Morgan and Travis were enjoying a morning at Terry Peak, getting in some runs down the mountain before celebrating a family birthday. They were headed down Ben Hur, one of the resort’s black diamond runs, when another skier cut Morgan off, leading her to veer left. “As I was turning, my skis got caught on one another,” Morgan explained. “I remember being super close to the ground and could feel myself flipping before I got knocked out, but honestly I don’t remember it in too much detail.”
For Travis, the crash — which he referred to as the worst moment in his life — was burnt into his memory. “When she got her skis crossed, one popped off right away and she cartwheeled, hitting her head. I was trying to get stopped, but was already farther down the hill at that point, and I didn’t realize at the time that she went off a 15-foot berm and hit a tree. I heard the impact, but even then I didn’t realize how bad it was,” he explained.
Getting himself stopped, Travis began yelling to his daughter, but received no response. As he was making his way back up to where she had crashed, a man yelled to him that she was unconscious. Morgan woke up face-to-face with that skier, and she vaguely recalls her dad approaching her.
“When I got to her, she had blood coming out of her nose, her face was scratched up and she had a pretty significant black eye,” Travis said. “I asked her, ‘are you okay?’ and she told me that her back hurt really bad.”
Travis asked her if she could move her feet, and she said that she couldn’t. “I could see that she actually was moving her feet when she answered, but the fact that she didn’t feel herself doing it, well, I knew that was bad,” he said.
Once Travis had reached Morgan, the skier that had first responded to Morgan’s accident and tried to wake her put his skis back on and rushed down the mountain, racing to the lodge to alert ski patrol.
Getting off the slope
Ski patrol arrived on the scene and got to work immediately. Because of how Morgan had landed, they had to take extra care to extract her — she wasn’t lying on flat snow, but in a depression that was full of undergrowth and branches. Over the next 15 minutes, ski patrollers used backboards to support and eventually lift Morgan while keeping her neck and spine protected. She was loaded onto a sled connected by fixed arms to a member of the ski patrol who brought her down the slope.
At the base of the mountain, an ambulance from Lead-Deadwood was waiting. EMTs loaded Morgan into the ambulance and ferried her to Monument Health Lead-Deadwood Hospital. “I don’t remember too much from the ambulance ride, but I know they gave me something for the pain and that was a relief,” Morgan said. “Everything got a little fuzzy, but I felt better knowing I was headed to the hospital.”
“Ski patrol are the people who are here to help you when you’re in trouble. Everybody has medical training — we’ve had EMTs, paramedics and even some nurses and physician assistants. There are some wilderness first responders that can help with some rescues,” said Chris Spellmeyer, SkiPatrol Director at Terry Peak. “We don’t just help with medical emergencies and evacuations though. We help when group members get separated or kids get lost, or even when people lose equipment or gear. We inspect the slopes to make sure they’re in good condition. The number one thing is that we’re here to help, no matter what the problem might be.”
Lead-Deadwood Hospital
Morgan may have been off the mountain and headed for a hospital bed, but as she soon learned, she wasn’t out of the woods yet.
“When we got to Lead-Deadwood Hospital, I felt a lot better about everything,” Travis said. “Everyone was putting me at ease, reassuring us that everything would be okay. The interactions were lighthearted.”
Morgan was given a CT scan to better assess her injuries, and when the results came back, the tone of conversation shifted dramatically. “Things went from light and jovial to all business. They told us this was out of their purview,” Travis said. “They said that there was a significant fracture along her spinal cord, and they weren’t equipped to handle it there.”
Morgan was loaded back onto an ambulance and transferred to Monument Health Rapid City Hospital where she was taken to a room in the ICU. “Based on what was visible on her CT scan, we knew that there was a serious fracture of the spine,” said Neurosurgeon Kyle Schmidt, M.D. “To get a more thorough picture of the injury, we ordered an MRI. This showed that while the vertebrae were fractured, they were still where they were supposed to be, and we saw no signs of damage to the spinal cord.”
The prognosis was good — Morgan’s spine could heal itself, she just needed time.
“She was only 17 years old — she was still growing. That’s why her spine could repair itself,” said Dr. Schmidt. “If a fully grown adult had these injuries, they would be in surgery immediately and have screws, pins and rods in their back for the remainder of their life. Because her bones weren’t fully formed, we rightly believed that a
custom brace could support her while she healed.”
It took two days to complete Morgan’s custom brace, and once fitted, Morgan was able to take her first literal steps toward recovery. “With the brace on, they had me walk down the hallway and walk up and down stairs to make sure I could handle it. And they said, ‘Oh you can do this, no problem, I guess you can go home tomorrow.’”
Home again, home again
Morgan was happy to return to the comfort of her home, but it came with its own challenges. There was very little she could do without putting the brace on. In fact, there was only one thing she could do — lie still. Any movement, from reaching for a drink of water or trying to sit up, required assistance putting the brace on.
“I think I’ve always been pretty independent,” she said. “And to be 17 and need help doing anything — even just getting out of bed — was pretty hard for me.” She was restricted from lifting anything over 10 pounds, as well as any heavy physical activity. “I couldn’t stand up, sit down or lie down for more than 30 minutes at a time,” she added. “So there was a lot of putting the brace on and taking it off to lie down and then getting back up again.”
She was also in a lot of pain, especially during the first few weeks back home. Muscle relaxers took the edge off, but they didn’t erase the pain. The only thing Morgan could do was bear it. In time, the pain lessened, although she still experiences some discomfort to this day.
For four long months, she wore her brace. Normally an active, independent teen, Morgan felt like the time dragged on and on, but Dr. Schmidt’s plan worked. Regular CT scans at Spearfish Hospital showed that her spinal fractures were healing and that her back was staying properly aligned.
“I was out of the brace, which felt so good. But I’m not free and clear to do whatever I want yet,” she said. Morgan’s activities are still restricted, but not for long. “Right now, I’m basically limited to walking. By April, I should be able to get back to doing what I like. I can even start skiing again if I want to. Whatever I want.”
She has enjoyed getting back to her normal life. She missed a semester of school while she was recovering in
her brace, so she’s been playing catch up since she returned. “It had been eight months since I had been in school. I was nervous that I wouldn’t be able to get back to where I’m supposed to be, but I caught up and I’m on track to graduate on time,” she explained. She has also returned to her job at Blackbird Espresso, which she enjoys, although being on her feet for long periods of time causes back discomfort at times.
Morgan has also been thinking about getting back on her skis. When asked if she plans to hit the slopes again, Morgan didn’t hesitate. “I still love it and I want to go skiing. I’m sure I’ll get to the top of the hill and be afraid to go down, but I’ll do it anyway.”
“She doesn’t really have a lot of quit to her,” added her dad, Travis. “If she wants to ski, she’s not going to let this experience keep her from doing it. After all this, I think whatever she wants to do, in any aspect of life, she won’t let anything stop her.”
Story by Wade Ellett
Photos by Bob Slocum
When you’re experiencing a medical issue and you don’t know if you should schedule a primary care appointment, go to urgent care or head directly to the emergency room, triage call nurse Grace Hastey, RN, BSN, knows just what to ask: “We use proven protocols that we go through. We ask a lot of questions, and it’s very patient specific.”
For Grace, serving as a triage call nurse is a family affair. Growing up in Colorado, her mother set an example as a triage call nurse, and although Grace didn’t necessarily intend to follow in her mother’s footsteps, she quickly fell in love with the profession and the advantages of working the phones. “It never occurred to me that I’d be doing this,” Grace said, but as she also pointed out, “I’m a talker… and this is a super valuable tool for the community.”
The program got the green light at Monument Health in June 2021. At first, they were helping patients manage COVID-19 symptoms, schedule diagnostic testing or vaccines. Now, the program has evolved into addressing a variety of issues — from refilling prescriptions to following up on discharged patients.
“I work with an amazing team from incredibly varied backgrounds. We have nurses that have previously specialized in OB, Urgent Care, ED, Cardiology, Ambulatory/Clinic and Wound Care just to name a few. We each bring something specific and unique to the team, but I have never worked with such a well-balanced team. We each work on specific tasks throughout the day, but everyone is so helpful and each person is cross-trained to do every task. If one person is having difficult calls or situations, anyone else can jump in and help out, and they all do so willingly, often without being asked. They see the need and fill it.”
“My role as a telephone triage nurse involves assessing any variety of conditions over the phone and helping the patient get to the right level of care at the right time. We follow evidence-based protocols that are very conservative to accomplish this — between pediatrics and adults there are almost 700 protocols to assess,” Grace explained. “We triage anything from snake bites to sore throats, blood pressure issues to poisoning, vomiting to foreign bodies and almost everything in between. If someone can be seen appropriately in the clinic in the next day or so, we will recommend some things to try at home in the meantime, and if they need immediate care, we connect them with emergency services or direct them to the ER.”
The Nurse Triage Line team fields calls from other clinics, but they are a free service readily available to the community. “Anyone can call us when they have a question about what care they need. We get between 1,600 and 1,800 calls each month, and we divvy them up depending on the need,” Grace said. The nurses spend about 10 minutes on each call.
Stomach pain, vomiting and diarrhea are among the most common complaints. Grace emphasized that they provide patient-centered care, even though it’s not in person. “I’m really glad I’ve been able to help bring this to the table.” Grace said. “I just wish that the community at large knew we’re here, and we’re available. This is a free service, and if you want to talk to a nurse about what’s going on and get an educated assessment of what’s going on, we can do that for you.”
Each day is different, and you never know what questions callers will have. One of Grace’s most memorable calls came from someone visiting from out of state who was bit by a prairie dog in the Badlands. “I used the ‘animal bite protocol’ and sent them in for rabies exposure and potentially rabies prophylactic treatment.” And there’s no judgment, she said. “I didn’t ask what they were doing. It wouldn’t have changed my advice.”
“I’m passionate about helping people, which is why I was drawn to nursing in the first place. By transitioning to telephone triage, I am able to help so many more people than I could working in ICU and just having one or two patients per shift,” Grace said. “Don’t misunderstand me, that is absolutely vital work, but I found myself in a season of life where I needed to have more emotional space and telephone triage was an asset for me and a wonderful shift in dynamics. I’m grateful that I get to do one call at a time and focus on that one person, and once I’m done I can move onto the next one. It makes me more mentally present for each call.”
Story by Stacy Friedman
Photos by Bob Slocum
Some people have a certain charm about them — people say that they light up a room, that their smiles are contagious or that they’re just fun to be around. Elizabeth Sterling is one of those people.
She works at Monument Health through Black Hills Works, putting together med bags and hygiene bags, as well as IV kits at times. At age 29, she’s been at it for seven years, and she still enjoys it. “I like getting things ready for patients at the hospital,” she said.
Elizabeth was born with a small deletion on one of her chromosomes that caused some cognitive impairment, but she hasn’t let it slow her down. “She’s happy, and productive and loving life,” said her mother,
Melinda Sterling. In addition to loving her job, Elizabeth has participated in the Special Olympics many times, and has especially enjoyed bowling and track.
When it comes to having fun, Elizabeth is a pro. She enjoys hiking, cycling and music — with a special appreciation of country music and classic rock — and loves going to concerts when she can. “People enjoy being around her,” Melinda said.
Elizabeth has type 2 diabetes, which she manages with Ozempic, a medication taken once a week by injection. The medicine works by increasing the amount of a hormone called incretins in the body, helping it to make more insulin when needed. It also reduces the amount of glucose made by the liver. She monitors her blood sugar on a regular basis and doesn’t have to take insulin.
Because of her diabetes, Elizabeth sees board-certified Endocrinologist Sonalika Khachikian, M.D., on a regular basis. A trip to the doctor may make some people nervous, but not Elizabeth. Her relationship with Dr. Khachikian, or Dr. K as she sometimes refers to her, has grown beyond just a doctor-patient interaction into a friendship. “Dr. K is so nice,” explained Elizabeth. “I feel like I can talk to her about anything, not just my diabetes or health.”
“She makes Elizabeth feel important. She asks her questions directly instead of asking me all the questions,” explained Melinda. “And she asks about her life, what she’s up to, about her job. She never rushes, and she treats Elizabeth like a whole person, not just a patient.”
This relationship isn’t one-sided — Dr. Khachikian enjoys their visits as much as Elizabeth does. “She’s such a sweet, lovely person. Some may consider her shy but she just needs a moment to open up. She’s kind and enjoyable to speak with, and I look forward to our appointments,” said Dr. Khachikian. “She always greets me with a hug and a smile, whether we’re in the office or if I run into her out and about — at T.J. Maxx or a local theater — she never hesitates and always makes a direct line to give me a hug. Elizabeth is a joy.”
Black Hills Works
is a person-centered agency that helps individuals with disabilities set goals and provides education, experience and support as they work hard to achieve them. Monument Health is proud to partner with Black Hills Works, and is the largest private employer that partners with the organization.
To learn more, visit
blackhillsworks.org.
Elizabeth and her family have managed her diabetes since she was a teenager, so she’s no stranger to monitoring her blood sugar levels and her weekly Ozempic shot on Fridays. Type 2 diabetes is progressive, so she may need to change up her treatment in the future, but for now she isn’t worried. She knows that her friend Dr. K will help her tackle any changes.
“Honestly, she’s a wonderful patient. She listens, is attentive and tries her best to answer any questions I may have. We have a great rapport,” said Dr, Khachikian. “It's nice to see how much her family cares and how involved they are in her overall health. Even with her unique disability she is able to engage and be involved in her overall health plan. She, like any other patient, has her preferences and I think it is imperative to respect those wishes. Elizabeth's sweet personality is just the icing on the cake.”
Lots of people are afraid to visit their doctor, put off tests and visits or never establish relationships with the individuals who provide their medical care. “Forming a strong, safe relationship with your patients is the window to excellent care. It really empowers patients to let their guards down and address their true concerns with their provider. This helps to strengthen the doctor-patient bond and may even spark a friendship,” said Dr. Khachikian. “I’m grateful for my friendship with Elizabeth and her mother. They are always a bright spot in my day.”
“Not everyone can say they’re excited to go see their doctor,” said Melinda. “But for Elizabeth, a visit to Dr. Khachikian is always a treat.”
“I’m already looking forward to our next appointment,” added Elizabeth.
Story by Wade Ellett
Photos by Bob Slocum
Spend time with Monument Health’s caregivers and physicians, and it’s obvious that there are plenty of gifted individuals throughout the organization.
The skills and abilities they use to help patients and one another are second to none, but everyone who participated in the recent Monument Health Has Talent competition showcased a different side of themselves; and a different kind of talent.
Nine finalists from across the organization performed in a December finale show, having advanced from three preliminary events held in Custer, Spearfish and Rapid City.
Anna Simons, a Registered Nurse at Monument Health Sturgis Urgent Care, was awarded first place as a solo vocalist and guitarist. Second place went to General Surgeon Pial Hope, D.O., who played the tabla — a North Indian percussion instrument. Sandra Walby, EVS Director for the Northern Hills, won third place as a solo vocalist.
In addition to showcasing the artistic talents of Monument Health caregivers, the competition also raised money for the Monument Health Foundation.
The open-to-the-public preliminary events saw dozens of caregivers from across the Black Hills show off their talents for a good cause, and ticket sales benefited the Foundation. Each first round event saw local celebrity judges send one contestant to the final, with the crowd choosing a second finalist.
“For the first year of this event, I'd say it was an incredible success,” said Hans Nelson, Director of the Monument Health Foundation. “I was so pleased to see over 25 caregivers register who were willing to get up on stage and share their talents, and I was shocked by the different kinds of talents on display. We had different styles of instrumentalists, vocalists, fire dancers and silk ribbon aerialists.”
1st Place - Anna Simons, RN
Simons’ winning performance was a rendition of Leonard Cohen’s “Hallelujah” with her own deeply personal lyrics. “I've been singing since childhood. My mother is an incredible guitarist, so I was usually singing along with her.”
It was Simons’ mother who gifted her first guitar as a stress reliever when her daughter was in nursing school. Since then, Anna has sung and played live with bands and on her own. While her connection to music has fostered positive personal growth, the lyrics she sang in the competition came from a more complicated emotional wellspring. She dedicated her performance and wrote the lyrics in memory of her brother, Sgt. Michael Simons.
“Mike served two combat tours in Iraq and suffered for years with PTSD, alcoholism and disordered eating,” Simons shared. Mike died from heart failure in 2015. “Losing him was devastating. I wanted to tell his story, so I decided to re-write the lyrics to "Hallelujah" in his memory. It is just such an emotional song. The original lyrics talk about love, but they also have this darker thread that speaks about the deep suffering that sometimes happens when you love someone. I think a lot of people connect with that, and it’s very humbling to win the competition singing this song.”
2nd Place - Pial Hope, D.O.
Dr. Hope is relatively new to Monument Health, as he joined the organization late last year. A General Surgeon specializing in metabolic and bariatric surgery, Dr. Hope made his presence known in the competition when he first played his tabla. The tabla is a pair of hand drums that has been the principal percussion instrument in Hindustani classical music since the 18th century.
Hailing from Los Angeles, Dr. Hope has been playing the tabla for 25 years.
“It provided me with discipline and focus as a child and was an excellent outlet for stress. It was my meditation, my joy and at times, my escape,” Dr. Hope shared. “It gave me the opportunity to see many interesting and talented people from a myriad of backgrounds and provided me with tremendously enriching experiences.”
Dr. Hope’s finale performance drew the crowd in as his fingers struck different points of the drum heads to produce different tones. His solo laid down a rhythmic bed of percussive notes and introduced many to the tabla’s sound.
“I love that rhythm is universal, which allows for unrestricted collaboration across genres. The rhythm I am able to produce with the tabla transcends culture and language, which is wonderful.”
3rd Place - Sandra Walby
A singer all her life, Walby brought some soul and southern charm to a rousing rendition of “Me And Bobby McGee.” Sandra said she was touched by the talent with whom she shared the stage.
“Singing just brings me joy, and I feel it helps people keep faith and stay strong when life is difficult,” Walby said. “Hold on to the good stuff like the talent you need to share to bring joy to yourself and other people. Monument Health is all about the patients and the people. I am very blessed to work here.”
With the success of the inaugural event, the Monument Health Foundation has already announced the dates for the next Monument Health Has Talent search later this year — Oct. 15, 17 and 18. Hans is enthusiastic about the event as a new way for the Foundation to engage with the community.
“What I loved most about the event was that it highlighted our caregivers and physicians in a manner that humanized them and showed a different perspective outside of the clinical setting,” he said. “It was a unique way to bring us all together, a night to leave the scrubs, suits, schedules and clinical settings behind and be ourselves.”
Story and Photos by Bob Slocum
At large community events such as the Black Hills Stock Show, the Black Hills Pow Wow, YFS Kids Fair, the Central States Fair and the Lakota Nation Invitational, as well as smaller community health fairs, Monument Health helps people check their blood pressure, pulse and blood oxygen levels. Participants can also assess their risk for diabetes and anxiety.
These health screenings allow patients to make informed medical decisions and take action to improve their health. The screenings have uncovered early warning signs of potential health issues leading to timely medical intervention, thus preventing the progression of illnesses.
Kris Legner, PA-C, is a member of the medical staff at Monument Health Sturgis Clinic, seeing patients who live and play in the Black Hills. She shared some insight into what makes health screenings valuable to community members.
Join us quarterly at the Sturgis Community Center
Events include an annual wellness fair with community vendors and booths to promote and educate health and wellness.
Also, Community Health Talks will provide an opportunity to connect local residents with the public and private health-related organizations and medical professionals available in the Sturgis area. The goal is to educate and inspire patients to invest in their own health, ultimately promoting better personal outcomes and improving the well-being of the Sturgis community. Please join on the upcoming dates of April 11, Aug. 22 and Nov. 21.
Question
Is it important for people to know their baseline blood pressure?
Answer
Yes, as this vital sign can help provide a picture of the patient’s overall risk of cardiovascular disease. If hypertension is diagnosed and treated early, it reduces the risk of a stroke and heart disease.
Question
When is it important to discuss my results with my primary care provider?
Answer
There is a lot of medical information available to patients these days on multiple media options, and unfortunately some of it can be false or misleading. By meeting with a medical provider, the patient is given the most up to date medical facts and allows time for education to occur, helping the patient gain enough information to make important decisions about their short- and long-term medical treatment and management plans.
Question
What does our blood pressure, pulse and blood oxygen levels tell about our overall health?
Answer
These vital signs give a glimpse into a person’s overall health and risk for complications. For example, high blood pressure leads to extra work by the heart. This extra work can lead to damage to organs like the brain, eyes and kidneys, as well as to the blood vessels.
Question
Do free health screenings replace annual physicals with a primary care provider?
Answer
No, free health screenings assist in finding health issues sooner, potentially making them easier to treat. The physical exam provides a complete head to toe assessment but also focuses on the patient’s risks.
A primary care provider also talks to the patient about sleep, diet and exercise
habits, offers age-appropriate vaccinations and any other screenings they may need.
It also helps develop a trusting relationship between a provider and patient for future medical concerns.
As frontline ambassadors, these professionals orchestrate schedules, insurance, billing, gathering demographic information and more to make sure the symphony of medical practice and procedure is carried out efficiently and effectively. Even more so, the Patient Access Specialists are the first people patients talk to when scheduling or checking in to their appointment.
“My role with Monument Health is making a difference every day,” said Darienne Jahner, a Patient Access Specialist for Urology at Rapid City Clinic. “I want patients to receive the care they deserve from the moment they walk in the door.”
Darienne Jahner grew up in Rapid City and admires the community that has evolved and advanced over the years. If she isn’t hanging out with her close-knit family, she is often at events throughout the area – especially events like the Turkey Trot and February Freeze 5K. Within Monument Health, she is known for her lasting relationships with patients, physicians and caregivers.
Throughout her career, Darienne has held a variety of positions in customer relations – from coffee shops to restaurants. The common thread among them all is the connection and care for others. When her friend brought forward the opportunity to join the Monument Health team, it seemed like a perfect fit. Now, two years later, Darienne is making a difference in her department, as well as patients’ lives through every interaction she has.
“I make a point to try and be on a first name basis with each of our patients. It seems small, but when you’re able to talk with someone and remember their names, I feel like it helps calm them for what may be a stressful appointment,” said Darienne.
No matter what kind of day Patient Access Specialists are having, they put their responsibilities first to make sure everything for the day of appointments will run as smoothly as possible. Darienne and her team make sure the waiting rooms are tidy, prepare medical staff for the day ahead and ensure time frames are filled and on schedule throughout every visit. Outside of internal communication, the Patient Access team will have a variety of duties that change from one day to the next. These tasks can include making calls to patients as a reminder of appointments, rescheduling as needed, following up on concluded appointments patients have had and more.
“I want patients to receive the care they deserve from the moment they walk in the door.”
-Darienne Jahner
“I think one of the most unique things about my role as a Patient Access Specialist that someone outside of the medical field may not realize is the amount of background work that takes place to make sure appointments are getting made and time frames are filled appropriately. It’s always changing, and it’s an important job to navigate that,” said Darienne.
With change comes challenge, and that is something Darienne is always up for. With a passion for personal and professional growth, Darienne has been taking the steps to build on her education in the health care access field. Through opportunities presented by Monument Health, Darienne accepted the chance to prepare for a nationwide exam to become a Certified Healthcare Access Associate.
“Monument Health has a great training program that can go as far as you want to take it. They give you support to advance in this profession, and knowing that I will be able to one day reach more leadership roles and administration tasks is encouraging,” said Darienne.
The team of Patient Access Specialists are a close group that works together to make patients feel at ease while also showing them they are receiving the best possible care. The team is supportive, always ready to help and step in for each other – encouraging growth and becoming the best version of one's self. From group training and team updates to potlucks and get togethers outside of work, the Patient Access team is a community within the frontline itself.
It can be uneasy for patients to visit the doctors. There are countless directions of diagnoses and treatment plans, and the anxiety that may come with that can be disrupting. Thankfully, being greeted by and working with caring professionals like Darienne at the very beginning of your care can make all the difference.
Story by Jenna Carda
Photo by Bob Slocum
Jim Phillips has probably spent as much of his waking life outdoors as indoors. He coached baseball, track and swimming in the Lead-Deadwood area. Now retired, he loves biking, kayaking and tending to his five-acre homesite in Boulder Canyon. Plus, Jim is an avid swimmer. In the summer of 2018, he and a friend swam across all 23 lakes in the Black Hills – 26.6 miles total.
“All my life, I’ve kind of been a sun worshiper. Back in my era, sunscreen wasn’t a big deal,” he said. “I’m 78, so that’s how many years I’ve abused the heck out of my skin.”
In fact it was swimming that made him aware that a spot on his nose, right where his swim goggles sit, would not heal. “I’d get done with a race or something, and I’d be bleeding from my nose,” he said.
Over the years, Jim has undergone various treatments to remove precancerous and cancerous growths. But this time it seemed more serious, Jim said. And it was. At Monument Health Dermatology in Spearfish, he found out the spot was basal cell carcinoma.
It’s a type of cancer that begins in the basal cells, the part of the epidermis that constantly makes new skin cells and pushes them to the surface. A DNA mutation causes the cells to multiply rapidly and continue growing instead of dying off to make room for new healthy cells. Chronic sun exposure, radiation therapy, fair skin and increasing age are among the primary risk factors.
The good news is that Mohs surgery is an extremely effective treatment for skin cancer. It’s known for a high cure rate and tissue-sparing results. Dermatologist Christopher Gasbarre, D.O., at Monument Health Dermatology in Spearfish, is a board-certified dermatologist and Fellow of the American College of Mohs Surgery. This year, he was joined in the Spearfish clinic by Mary Logue, M.D., a dermatologist who is also board-certified in the procedure.
Mohs surgery is an outpatient procedure. The tumor and a small amount of surrounding tissue are surgically removed. While the patient waits, the cells are sliced, mapped and examined under a microscope. If the layer has cancer cells, another layer is removed, then examined in the same way. When all of the cells in a layer are clear of cancer, Dr. Gasbarre closes the wound and sends the patient home to heal.
“Because Mohs surgery removes the least amount of healthy tissue, patients are left with smaller, more manageable wounds,” Dr. Gasbarre said. “For this reason, Mohs procedures work especially well on areas of the body in which sparing tissue is important, such as near the eyes, ears or nose.”
In Jim’s case, the tumor site on his nose is practically invisible today. He had the surgery on Jan. 3 at the Monument Health Dermatology clinic in Spearfish. It took about three hours.
“Three hours was nothing. I had a basketball game on TV, and I took a nap,” he said. During the surgery parts of the procedure, he chatted comfortably with Dr. Gasbarre, Certified Nurse Practitioner Darbi Anderson and other staff members about everything from liver and onions to the difference between aerobic and anaerobic exercise.
These days, Jim is a big believer in taking care of his skin. He still spends a lot of time outdoors, but he’s using lots of sunscreen. When he’s out doing yard work, he wears his favorite Chicago Bears baseball cap.
“And my wife got me some cream that makes my skin look like it’s only 75 years old now,” he added with a chuckle.
Story by Dan Daly
Photos by Bob Slocum
It was just another day at work for Danny Morris.
The Monument Health valet supervisor was at his usual place near the entrance to Rapid City Hospital, greeting people and talking baseball with his coworkers.
Little did Danny know, a blood clot that started in his leg was moving into his lungs. One moment he was running down the Chicago Cubs batting order, the next he was unable to speak and began struggling to breathe. When he hit the floor, he was in cardiac arrest; suddenly fighting for life in the very same spot he’d been working for the last 24 years.
“All of a sudden, I couldn’t answer them when they asked if I was OK,” Danny said. “I woke up in the ICU a few days later.”
Gary Dowling and Dale Johnson, fellow valets, immediately called for rapid response. Heart and Vascular Unit nurses Cori Johnson, RN, and Amy Farley, RN, were only a flight of stairs away and headed straight for the scene. They began lifesaving measures within seconds of hearing the call. Cori and Amy took turns giving Danny chest compressions and instructed Gary and Dale to call for a code blue. The code blue team quickly arrived and Danny, still unresponsive, was loaded onto a cart.
At that point, Amy climbed onto the cart with Danny and rode with him, administering CPR as they were wheeled to the emergency department. Treatment continued in the ED until Danny resumed breathing and was eventually stabilized.
“I have responded to more codes than I can count over the years, but this one had an impact on me,” Amy said. “I think since it was a colleague — one of our own — it has stuck with me over the last year and probably will for the rest of my life.”
The close proximity to care when it mattered most was a factor in Danny’s case, Cori said.
“I knew Danny had an excellent chance of full recovery because CPR began when he became unresponsive and lost his pulse,” she said. “It does feel more personal when you know the person you are helping. This has happened to me several times over the years both at work and in the community. The first time I saw Danny when he returned, I shook his hand and told him how glad I was to see him and told him Amy and I had been praying for him ever since.”
What is a code blue?
A code blue hospital announcement means that an adult is having a medical emergency, usually cardiac or respiratory arrest. Every hospital has its own policy for code blue events. Cori Johnson, Nurse Manager at HVU, said “I have been a nurse here for almost 33 years, so I have responded to hundreds of code blues over the years. Each one is different, but the feeling of urgency and desire to help the person with all you have is the same.”
From the ED, Danny was sent to the Intensive Care Unit for several days where he was on a ventilator. Danny's wife, Deb, and daughter, Brittany Pruess, were by his side for support. He was treated by Cardiologist Saverio Barbara, M.D., Samantha Speed, DNP, and others at Monument Health Heart and Vascular Institute.
Five weeks after nearly losing his life in the middle of his shift, Danny walked back into the valet office and resumed work.
“I’ve always said I like working here, and I do. That’s why I’ve been here so long; I enjoy it, and I’ve always thought of my teammates as a family,” Danny said. “Well, they truly are my family now, because I owe them everything.”
It’s been a year since his incident, and Danny has been doing what he always has: parking cars and helping patients and visitors. He’s seen the arrival of a new grandson, Nehemiah James Pruess. The Cubs are entering spring training, and the guys are starting to talk baseball again. Dr. Barbera gave him an implantable cardioverter- defibrillator, a small battery powered device placed in the chest. It detects and stops irregular heartbeats, just in case something like this should happen again.
“I feel good,” Danny said. “I’ve been treated so well by everyone here at Monument Health, from the ED to ICU to HVI; all the doctors and nurses and everyone else. Gary and Dale helped me on the spot, and then our whole team stepped up and filled in while I was gone. Everyone just takes these things as part of the job around here, but for me, it’s a lot more than that. It means so much, and I just want to thank everyone who helped me.”
Danny’s role as valet supervisor puts him in constant contact with Monument Health’s patients. Often, the first Monument Health caregiver a patient or visitor sees when they arrive at Rapid City Hospital is one of the valets. On an average month, the valet services team parks and retrieves 2,800 vehicles and helps more than 2,100 patients — including wheelchair assistance when required. Danny said the entire valet team takes pride in making arrival and departure less challenging for patients.
“They truly are my family now, because I owe them everything.”
-Danny Morris
“The goal is to make patients and visitors feel like VIPs,” Danny said. “Our team is committed to providing positive experiences.”
He still thinks about that “scary and remarkable” day each morning when he arrives at the hospital. “It’s not to be forgotten,” he said. “It’s to be acknowledged, so that the healing can foster a grateful outlook.” Danny has been well known around the hospital, but he’s now earned a new nickname from those who know his story: some call him Miracle Man.
“It could have happened anywhere. The Big Guy, he put me in the right place with the right people. You truly know who’s beside you when something like this happens.”
Story and Photos by Bob Slocum
Rapid City Hospital is home to two specialty coffee cafes: Market Coffee and create. Each serving Starbucks drinks, breakfast and lunch to caregivers, patients and visitors. The team behind the counters is dedicated to providing fast, friendly service to everyone who stops by.
Chanwanpe Shields started as a barista in March 2023, and she brings her personality and individuality with her to work every day. “If I was to introduce myself, I would say I’m Lakota Dakota, from Marty, South Dakota, and an enrolled member of the Yankton Sioux.”
“I love to share about my culture,” she said. “I feel like that's one thing about my identity that I'm always willing to share is where I come from — I’m surrounded by my culture with modeling and with my volunteer work. It's all for the community here.”
There are many regulars who stop to see Chanwanpe and her team at both cafes in Rapid City Hospital. She enjoys seeing patients progress along their healing journey. “There was one patient I remember seeing on crutches, and a few weeks later he was walking on his own — that was great to see.”
Each day the barista team works together to ensure an efficient and positive experience for their customers. Ask any regular at a coffee shop and they’ll tell you baristas don’t just create drinks — they get to know their customers well enough to start their order before they even step up to the counter.
“Being a barista isn’t just about coffee,” Chanwanpe explained. “It’s also food service. We have daily breakfast and lunch specials in create, and in Market Coffee we can go back to the main kitchen and help prep for lunch.”
create delivers an exhibition-style culinary experience where food is prepared right in front of you, with a number of options to customize your order. Open Monday-Friday, 6 a.m.-2 p.m., you can also find your favorite Starbucks coffee here, as well as a number of bottled beverages, grab-and-go food options and snacks.
Market Coffee provides an authentic café experience to caregivers, physicians and patients on the first floor of Rapid City Hospital. Open seven days a week, 7 a.m. to 11 p.m., baristas like Chanwanpe will serve your favorite cup of coffee with a smile. They also offer a seasonal menu with fresh gourmet pastries and grab-and-go items.
Service
Between the two locations, Monument Health baristas serve an average of 500 people each day. Sometimes their customers are ending long and challenging overnight shifts. Others are arriving to visit a loved one who is beginning a healing journey. Each of those 500 customers are treated with kindness and compassion.
“My team is like family to me. We all walk in with optimism. We lift each other up and put our heads together to improve the customer experience every day,” she said. “And every time we get to visit with someone, we strive to become a great part of their day.”
Chanwanpe doesn’t just serve her fellow caregivers at work. She also dedicates time to community service. “I started volunteering with my uncle when I was still in high school, and I still help him today when I’m able,” she said. “We serve meals at Memorial Park every Friday. Everyone is welcome: single mothers, single fathers, people in the community and especially our elders.”
Providing service to her community is important to Chanwanpe, and just like serving caregivers and patients at Rapid City Hospital, serving the community is a team effort. “I hope people driving by see the community that goes into the meal. It’s not just one family, it’s several families who are dedicated to always being there.”
A model for others
Service to others is important to Chanwanpe, and she hopes that others are encouraged to give back as well. “We’ve had people see what we do, and they’ve wanted to help as well,” she said. “I think when you serve others, you get back just as much.”
In addition to her service to others and work as a barista, Chanwanpe is passionate about modeling. She especially loves to combine that passion with her love of highlighting her culture and heritage. “Last April, I walked in two fashion shows — one was at the Dahl Arts Center and the other was at The Monument in Summit Arena, which is the biggest thing I’ve done,” she said. “It showcased native and indigenous artists, so I was proud to model their clothing.” Chanwanpe enjoys modeling, and it has led to new friendships in the fashion world. She is looking forward to more modeling opportunities and traveling in the future.
Community
Chanwanpe has a lot of sides, interests and passions, but the thread running through them all is community. “I’m always surrounded by community. Whether I’m modeling, volunteering or even when I’m at work, I’m always connected to my identity, my culture and my community. Everything I do is connected to that, and I try to bring the same passion and dedication to all the things I do,” she said.
“My team is like family to me. We all walk in with optimism. We lift each other up and put our heads together to improve the customer experience every day.”
CHANWANPE, ON THE IMPORTANCE OF TEAMWORK AND SERVICE TO OTHERS
Written by Stephany Chalberg
Photos by Bob Slocum
My Role
As a certified family practice nurse practitioner, I provide primary care for patients of all ages, managing chronic conditions and promoting wellness through education and prevention. I’m passionate about improving my patients’ quality of life and empowering them to be active participants in their own health.
My Goal
I strive to provide high-quality medical care to the people of Hot Springs and the surrounding area. We see patients from Nebraska, Pine Ridge, Buffalo Gap, Edgemont and even from Wyoming. I grew up in a rural South Dakota community and understand the challenges and benefits of providing care in this type of community.
My Passion
We are an hour away from Rapid City, so it can be very difficult for people to travel there for appointments. This is why I’m passionate about providing care in a rural
setting. As the Diabetes Champion at Monument Health Hot Springs Clinic, I provide a diabetes clinic with a Certified Diabetes Educator twice a month. My goal is to help people with diabetes experience a high quality of life with a disease that requires constant monitoring. Any chronic disease can be overwhelming, and my goal is to help people lead lives they enjoy, instead of letting the disease rule their life.
"I enjoy teaching the next generation of nurse practitioners. My patients have been gracious enough to allow these students to learn in nour clinic. I have provided over 2,500 hours of precepting to these students, and have found it very gratifying."
My role
I am a cardiologist at Monument Heart and Vascular Institute with a primary focus in cardiovascular imaging. I grew up in Rapid City and did my medical and cardiovascular training at New York Presbyterian. Additionally, I did a year of advanced cardiovascular imaging with a focus on cardiac CT, structural echocardiography and cardiovascular MRI at Houston Methodist Hospital. I help manage cardiovascular patients at Monument Health in the clinic and the hospital as well as assist in the specialized imaging needed for the Monument Health Heart Failure team as well as the Monument Health Structural Heart team.
My goal
My goal is to provide the Rapid City community and our patients with the newest technological advancements in cardiovascular care and cardiovascular imaging. I strive
to continue to learn and evolve as a physician and a
cardiologist so that I can provide our community with the most appropriate and optimal care. I hope to help the cardiology practice in Rapid City evolve and grow so that patients can receive their care close to home.
My passion
My passion is serving people in their greatest time of need. Cardiology provides an opportunity to help people in their most vulnerable moments in the hospital and then help and support them as they work to improve their heart health once they go back home. I am eager to contribute my skills and dedication to make a difference in the lives of those facing cardiovascular challenges, and feel fortunate that I am able to do so.
Dr. Ameer focuses on advanced cardiac imaging. This specialty refers to sophisticated techniques and technologies used to obtain detailed and comprehensive images of the heart and surrounding structures. This includes:
- Cardiac magnetic resonance imaging, which provides detailed images of the heart anatomy and function using
- a strong magnetic field and radio waves.
- Cardiac computed tomography, which uses X-rays to create cross-sectional images of the heart, allowing for detailed visualization of the coronary arteries and other structures.
- Echocardiography, which uses sound waves to create images of the heart and provides real time information about structure and function.
- Nuclear cardiology, in which a small amount of radioactive material is injected and used to assess blood flow and function of the heart muscle.
Lori Allen has struggled with breathing and other health issues all her life. Eventually, she was diagnosed with a heart condition that could only be corrected with surgery. As part of her follow-up care, Lori’s caregivers at Monument Health continued monitoring her cholesterol levels post surgery. “My cholesterol has always kind of been a big thing,” Lori explained.
Knowing that Lori’s cholesterol levels met certain special criteria, Bhaskar Purushottam, M.D., FACC, FSCAI, FSVMB, reached out to Monument Health’s Clinical Research department to see if Lori would be a good fit for an upcoming clinical trial.
Being a part of clinical research
Kelli McIntosh is the Director of Monument Health’s Clinical Research department. She said that this lesser-known but crucial facet of the Monument Health system is vital in keeping caregivers on the cutting edge of treatment options. Sometimes, though, inviting patients to participate in a research study can involve overcoming some preconceived ideas. “The first thought that the general public has a lot of time is, ‘Well, I don't want to be a guinea pig,’” she said.
Roger DeRaad, CNP, Clinical Research Investigator, agrees with Kelli. He said that most patients are initially skeptical of participating in clinical research, but that many of them decide to join a study because of the benefits. “A lot of our patients mention that they're doing this for their family, for people in the future or to have a chance to fight back. It can be frustrating when you get a diagnosis, and sometimes patients just want to be able to do something,” he said.
Kelli, Roger and the whole team of Clinical Research caregivers advise taking advantage of an opportunity to participate in a clinical trial if you’re ever presented with one. As Roger described, there are many motivations to participate, but one outcome that might be surprising. “Participants in clinical research typically fare better than patients who are not,” Roger said. “It’s not necessarily because of the treatment, although it certainly can be beneficial. Often it’s because these patients are under a heightened level of observation.”
A 25-year legacy
The Monument Health Clinical Research department has been a part of medical breakthroughs for over two decades. And because many of the caregivers at Monument Health play such an active role in these trials, when a new drug or treatment is approved, these experienced nurses and doctors are able to hit the ground running when offering these new breakthroughs to their patients.
A life-saving discovery
Lori’s introduction to the Clinical Research team started in a typical way. “I got a call and I thought, ‘What is this? It seems kind of scary,’” she said. But Lori soon discovered that participating in clinical research is special, and that it’s about inviting a larger group of caregivers around you and your diagnosis. “Everybody that I've met through the research and all my doctors over at the hospital have just been super fantastic. I'm so grateful to everybody,” she said.
Lori’s participation in this clinical research study involved getting a Computed Tomography Angiogram, or CTA — a diagnostic test that she would not have received in her regular course of treatment. Because of that scan, Lori and her caregivers made a lifesaving discovery.
“If I hadn't had that CTA, I don’t know if I would still be here.” Lori’s CTA revealed an elevated chance of a heart attack that would have likely gone unnoticed if Lori wasn’t observed at that heightened level. “I'm very thankful for that. My doctor encouraged me to get into the research, and a part of the research was doing the CTA.”
Taking ownership of your own well-being can take many forms — exercising, eating right and staying informed. And sometimes it means, like in Lori’s experience, being intentional about surrounding yourself with the best caregivers you can find. Receiving a diagnosis can be scary, frustrating and even leave people with a sense of helplessness. Lori is living proof that you can fight back against those emotions. Participating in a research study — if the opportunity should arise — is one of those ways.
“Do it. It definitely changed my life,” Lori said.
Another pair of eyes
A reason caregivers were able to intervene early in Lori’s heart condition was thanks to Dr. Purushottam, who connected Lori with Clinical Research. If she hadn't participated in that trial, she likely wouldn’t have received the CTA scan that led to her caregivers performing open heart surgery. “Often patients are worried when they hear about a research trial, but in research, you have another pair of eyes,” said Dr. Purushottam.
Participating in clinical research proved to be vital in Lori Allen’s health — it may have even saved her life. “She could have had a major heart attack, which could have potentially killed her or led to heart failure,” said Charan Mungara, M.D., one of Lori’s surgeons. He was grateful to have been able to make a difference in Lori’s life. “She was an excellent patient,” Dr. Mungara added. “She’s a sweet lady and very appreciative. I'm glad she's doing well.”
Written by Stephen Simpson
Photos by Bob Slocum
Kip Wagner was 34 years old when he found out he had type 1 diabetes. His daughter, Katie Washnok, was diagnosed at age 12. Kip’s son, Kevin Wagner, was 25.
The Wagners are proof that genetics play a big role in type 1 diabetes. They also prove that the disease is not just a young person’s affliction.
“That's one of the misunderstandings about diabetes. We used to call type 2 diabetes adult onset and type 1 juvenile diabetes … but you can have young kids with type 2 diabetes and people in their 20s, 30s, 40s even 50s who get type 1 diabetes,” said Monument Health Endocrinologist John Palmer, D.O.
Kip, now 63, lives in Whitewood. He was referred to Dr. Palmer in 2011. “It took about 30 seconds to figure out I was in the right place,” Kip said. Now Katie, 34, and Kevin, 29, are also treated by Dr. Palmer.
“It’s a family affair for us with Dr. Palmer. My dad, who’s been type 1 for almost 30 years now, is the best testimonial out there for Dr. Palmer,” said Kevin, of Spearfish. When Dr. Palmer was practicing in Sioux Falls, the family would go to Sioux Falls for treatment. And Katie, who now lives in Aberdeen, travels across the state for her appointments with him.
During a recent interview at Rapid City Clinic, Flormann Street, where Dr. Palmer practices, Kip, Kevin and their doctor chatted about glucose levels, insulin units and basal rates with the ease and comfort of old friends.
Different diseases
Both types of diabetes involve problems with insulin, a hormone produced by the pancreas to regulate blood glucose — also called blood sugar — in the body’s bloodstream. It helps turn the food you eat into energy and store energy away when it’s not needed.
Not enough glucose in the bloodstream means you feel tired and weak. The body could eventually begin burning fat and muscle to keep going. Too much glucose can damage nerves, blood vessels, tissues and organs.
Type 1 diabetes, Dr. Palmer explained, is an autoimmune disease. The body attacks the insulin-producing cells in the pancreas, causing them to stop production. For Kip and Kevin, insulin production tapered off for about two years before stopping. For 12-year-old Katie, her pancreas shut down completely and quickly.
With type 2 diabetes, the body either doesn’t produce enough insulin, doesn’t metabolize it, or both. Although there is a strong genetic factor in type 2 diabetes, poor diet and lack of exercise are its main drivers.
There is little that type 1 patients can do to avoid the disease. Dr. Palmer said Monument Health has been involved in clinical trials of treatments to preserve the insulin-producing cells before the autoimmune system can do its damage.
Advances in treatment
What separates Kip’s early diabetes experience from that of his children are the advances in technology that make it much easier to manage. In 1995, when Kip was diagnosed, living with the disease required regular pin pricks, syringes and a carefully controlled diet.
Now, Dr. Palmer’s type 1 patients regulate their glucose levels via sensors and insulin pumps attached to catheters embedded in the skin. Both devices communicate constantly with a cell phone app that shows glucose levels and allows patients to manually adjust their levels if needed. In addition, the quality of the insulin manufactured today is better, Dr. Palmer said.
“You used to have to really direct your lifestyle around the diabetes. You had to eat at a certain time, take your injections at a certain time and if you didn’t, there was trouble.” Dr. Palmer said. “Now your lifestyle becomes the focus.”
Still diabetes is a daunting diagnosis. That was especially true for Katie when she was diagnosed at just 12 years old. “It was tough, but I was lucky because I had parents who never let me have a pity party,” she recalled. “They said, ‘Yep, you’ve got this and you are going to be in charge of it. It’s not going to be in charge of you. You’re the boss.’ I was like ‘I love being the boss, so let’s do it.’”
When Kevin was diagnosed in August 2019, sensors, pumps and cell phone apps made the disease easier to manage.
“I got lucky I never had to deal with any of that,” he said, referring to the pin pricks and injections that used to control a diabetic’s life. However, he said, diabetes still requires a constant awareness of your health. “I read somewhere that the average diabetic makes 180 more decisions a day about their health than the average person,” Kevin said.
“You still have to be captain of your ship,” Dr. Palmer added.
Written by Dan Daly
One way to get to know people is to learn what they love. Some love nature and the wild, others love books and warm mugs of tea. Nurses are a special lot — they love helping people feel better. That’s true of Wanda Schummer, RN, but she also has a special place in her heart for the City of Sturgis and the people that call the place home.
For almost 50 years, Wanda has worked at Sturgis Hospital. She’s called the City of Sturgis her home even longer. “I grew up in Sturgis, and I went to school here. We raised our kids here,” Wanda explained. “We did move into the country, but I consider Sturgis my hometown. I’ve got so many links to the people here, including the patients I’ve worked with over the years.”
"The Sturgis Hospital is just part of my home."
Hometown nursing
Wanda is a clinical resource nurse, which is a subspecialty of registered nursing with a responsibility for coordinating nursing staff and overseeing the care of specific patient groups. For Wanda, those groups are endoscopy and pain management patients.
“Once a week two surgeons from Spearfish come over and we assist them with endoscopy, and we do pain management with West River Anesthesiology,” Wanda explained. “We’ve done pain management for about 10 or 15 years now, and I really enjoy doing that. The patients see me over and over again, so they know me. You develop a relationship.”
“You’re helping them feel better and they appreciate it.”
“I’ve had the privilege of being a member of the committee that’s developing the history wall in Sturgis Hospital. As I reviewed old photos and newspaper articles, I remembered so much of what has happened with our small hospital and how it has grown over the years,” Wanda said. “There were changes, but the goal was always to provide services to our community. I have worked with so many physicians, staff and patients over the years and each one has impacted my life.”
WANDA SCHUMMER
Supporting Sturgis
Wanda has spent her entire adult life serving the health care needs of Sturgis. She graduated from nursing school in December 1973, and started her nursing career in her hometown immediately in 1974.
In every small community across the country, you’ll hear kids talking about getting out of town — but not Wanda. She’s always felt that Sturgis is where she’s supposed to be. Growing up, her family owned and operated a western store downtown, Bob’s Saddlery. She got to know her hometown and the people who lived there by working and playing in that store. “There were more businesses downtown then, and it seems like there are more coming back now,” she said. “I may not live in town anymore, but this is where I do my shopping. I’m not running to Walmart — I go to the stores here in Sturgis. I think that’s one way folks can really support their community.”
In many ways, Wanda is ahead of the curve. Downtown revitalization is a growing trend across the country, and more and more people are becoming interested in a local economy, whether that’s by opening their own business or by spending their dollars downtown instead of at big box stores or online. Wanda has seen a lot of changes over the years, but she’s happy to see some of that enthusiasm for local business returning to Sturgis. “I think a lot of people want to see businesses flourish in their community, and if you don’t support them they’re not going to be here. To me, that’s a major problem.”
The times they are a changin’
It’s not just the community of Sturgis that has changed during Wanda’s tenure — the profession of nursing has evolved during her career as well. “If you go back to when I started, all of our records were on paper. We had a couple of nurses taking care of 20 to 25 patients, and we relied so heavily on our CNAs.” Wanda explained. “We did emergency surgery, we did deliveries. We did everything.”
In the span of her career, Wanda has had the opportunity to get to know her patients, and even to treat some
individuals who she helped deliver years ago, an experience that she has found both awe-inspiring and humbling.
“Sometimes you get to see the impact you’ve had, and that feels amazing. It’s always been for the community — offering services for the people here,” she said.
Sturgis Hospital itself has changed before Wanda’s eyes. She’s seen the hospital change hands from Lutheran Homes and Banner, to private ownership and finally Monument Health. “A lot has changed over the years, but one thing that hasn’t is how much our nurses and other caregivers care about the people here,” said Wanda.
What’s next for Wanda
Wanda still finds satisfaction in her work, and she still feels fulfillment in providing patient care. Likewise, Sturgis still feels very much like home, and she’s happy that she can continue to enjoy it with her family. “I have nine grandkids, and my second great granddaughter is due this year,” she said. “They’re the most important thing, and I’m grateful that they all live in the area.”
And although she’s reached the point in her career and her life where many people might consider retiring, and maybe even heading south for the winter, Wanda has no plans or desire to make those changes any time soon.
“I love my job. I love where I work. I have a really great community that I get to work for, and hopefully I can do my part to keep everyone here as healthy as possible.”
Written by Wade Ellett
Photos by Bob Slocum
There are many ways to describe Jamie Clark: licensed massage therapist, yoga instructor, kayaker, skier and camper.
While those may describe her hobbies and careers, they don’t necessarily describe her. To really understand who Jamie is, first you have to understand her quest for knowledge and her ability to touch the lives of others.
Oncology massage is growing in popularity as a complementary treatment for patients with cancer. The massage isn’t intended to treat the disease itself, but rather to help relieve cancer symptoms and ameliorate side effects of certain treatments. Despite its growing popularity, Jamie is the only massage therapist in South Dakota to be recognized by the Society for Oncology Massage as a preferred practitioner.
While it seems like a pretty specific niche, she didn’t start her career with a focus on treating cancer patients. Instead, it seems like the career chose her.
Between the yoga studio and the massage room at the Cancer Care Institute, Jamie hopes her spaces provide an opportunity for cancer patients to feel present and calm their nervous system. “These are also safe spaces for patients to express whatever they might be feeling,” she explained. “Whether they need to laugh or cry, these are spaces where they can let it out without any worry or judgment. Sometimes that’s exactly what someone needs.”
Open heart, open mind
“Right after I graduated from massage school, a client of mine said he had a friend that had a dual diagnosis of cancer and AIDS. He wanted to know if I would be willing to meet the patient. As a new graduate I was nervous, but I knew if I could just go and maybe sit with him, hold his hand and just listen, maybe that would be enough, because there is healing in that, too,” she said. “People need to be heard, touched and to feel connected.”
Jamie recalled the lessons she learned from that first client — treating people with an open heart and open mind can be just as important as massage techniques. “If I can help someone be comfortable even just for a few seconds, in their mind and in their body and just feel like they’re a whole person — even though they have this diagnosis — then I feel like I’ve become their helper.”
When Jamie first started her career, the recommendation was to not provide massage to cancer patients. The misconception, at the time, was that overstimulating the lymph system and increasing circulation in the body could cause the cancer to spread. Through her experience and certifications, Jamie has learned the safe way to massage cancer patients. She is aware of which areas of the body to avoid, and the pressure used is modified to ensure comfort.
“What we’ve learned in the last few years is that massage can be adjusted to meet the needs of each individual client. I always discuss their cancer journey with them before we begin.”
“If I can help someone be comfortable even just for a few seconds, in their mind and in their body and just feel like they’re a whole person — even though they have this diagnosis — then I feel like I’ve become their helper.”
JAMIE CLARK, ON HELPING PATIENTS UNDERGOING DIFFICULT DIAGNOSES
Considering compassion
Jamie considers her time with her clients in many ways. The more she understands their diagnosis, the better she can adjust her approach to increase relaxation and comfort to clients.
“The cancer journey is scary — it can be really hard and isolating for people.” Jamie realized that after a diagnosis, some people find friends or loved ones who don't know what to do or say, so they disappear from their lives. Jamie works to create a safe environment for each client to share as much or as little as they need. “Some days we laugh together until we cry together. Other days, clients and I will cry together, until we laugh. It doesn’t make everything better, but I can bring them just a little bit of joy.”
Being compassionate is part of who Jamie is, but she learned just how beneficial that compassion can be for patients facing significant challenges. “My mother had colon cancer, and when she got really sick and could barely speak we shared a mantra which was, ‘I’m okay today,’ and she would make the symbol of a heart with her hands.” Jamie also learned firsthand just how meaningful touch can be while she was there for her mom. “Sometimes she would ask me just to hold her feet — when neuropathy set in, that light touch might be all she could handle. Other times she asked me to rub her neck, shoulder, arms or hands. I really directed my attention wherever she needed it.”
Never alone
Jamie and the Cancer Care Institute team want to relay this important message to the people facing a cancer diagnosis: you’re not alone. There are resources and support systems in place to care for cancer patients. And, treating yourself to a massage may relieve more than just sore muscles.
“I’ve been doing this for over 20 years. I’m now treating more of the heart and the mind, not just the body. It’s not as hard physically, but I’m not gonna lie, some days, it’s hard
on my heart,” Jamie says. “But helping people feel better? It’s well worth the effort.”
The massage needs and physical abilities of cancer patients receiving treatment can be drastically different, so working with these patients requires specialized skills and training. On her quest to continue to learn, grow and improve her skills to care for her clients, Jamie is preparing for an additional yoga certification specifically to help instructors provide classes to those with cancer.
Written by Stephany Chalberg
Photos by Bob Slocum
What is heart failure, and how does it differ from other heart conditions?
Approximately 6.2 million adults in the United States are living with heart failure, which is a chronic condition where the heart is unable to pump properly so it can't meet the body’s need for blood and oxygen. Having heart failure does not mean your heart has failed or stopped working — it just isn’t working properly or as efficiently as it should.
Heart failure differs from other heart conditions like heart attack or arrhythmias because it’s a long-term problem. There are several potential causes, like high blood pressure, coronary artery disease, hypertension, heart attack or arrhythmia.
What are the common symptoms of heart failure, and when should I see a doctor?
The most common symptoms of heart failure are shortness of breath or trouble breathing, persistent cough or wheezing that’s prominent at night, an inability to sleep flat, leg swelling, fatigue and leg weakness, rapid weight gain, lack of appetite and nausea. If the heart function is especially low or inefficient, people may experience confusion, dizziness, trouble concentrating and even fainting. If someone experiences these symptoms, especially if they worsen over time, it’s essential to consult a health care professional.
What are the different types of heart failure, and how are they diagnosed?
Heart failure can be categorized into systolic and diastolic heart failure. Systolic heart failure, also known as reduced ejection fraction, is the most common type. In systolic heart failure, the muscle slowly weakens and loses the ability to pump blood. Because the heart is unable to pump enough blood, it typically grows in size while the muscle gets thinner. In diastolic heart failure, also known as preserved ejection fraction, the heart has lost the ability to relax normally because the muscle has become stiff. The stiffness leads to elevated pressures in the heart and lungs, which in turn prevents the heart from functioning as it should.
In these cases, the heart appears normal but with a smaller cavity and harder, thicker muscle, in varying stages of severity. Diagnosis involves a combination of physical exams, medical history, imaging tests and lab work to assess the heart’s function and
determine the type and stage of heart failure.
Can heart failure be prevented, and what lifestyle changes can help reduce the risk?
While heart failure cannot always be prevented, lifestyle changes like maintaining a healthy weight, managing blood pressure, thyroid problems, diabetes and cholesterol, exercising regularly and avoiding smoking can significantly reduce the risk.
How can heart failure be managed?
There are several medications that can improve heart failure symptoms and keep patients from being admitted to the hospital for heart failure. Most patients will require ARBs or ARNIs, beta-blockers, aldosterone blockers and SGLT2 inhibitors to treat their heart failure and sometimes we use diuretics to get rid of excess water. It’s important to understand that all of these medications work together. When taken properly, following the provider’s instructions, they will help strengthen the heart by reducing its workload, improving its pumping ability and managing fluid retention.
It’s also important for heart failure patients to manage their diet. This will include reducing
sodium intake, managing fluid intake and focusing on fresh foods, such as fruits and vegetables. It can be helpful to consult with a registered dietitian.
Similarly, exercise can be beneficial for individuals with heart failure, but it should be done under the guidance of a health care provider. Cardiologists can recommend safe exercises like walking, swimming or stationary cycling, tailored to each patient's needs.
Are there any new and innovative treatments for heart failure on the horizon?
There are exciting developments in heart failure treatment, including new drugs, advanced devices and gene therapies. Cardiologists with advanced heart failure training are well positioned to offer these cutting-edge treatments when appropriate, and provide guidance on the best options for each individual patient.
Photos by Bob Slocum
Monument Health Sports Performance Institute powered by exos, is dedicated to improving performance. For the clients that train there, this takes a lot of different forms. Some are Olympic hopefuls, others are preparing for their first 5K. There are professional athletes looking to advance their careers, and older cowboys training to stay in the saddle. The exos team provides performance training, nutrition services and an award-winning facility to help everyone who walks through the doors achieve their goals.
“When we say we want to help people accomplish their goals, we mean everyone, regardless of what that goal is,” said Kyle Wheeldon, General Manager of the Sports Performance Institute. “We’re used to helping with traditional athletic goals, but we aren’t going to put limits on what we do. If someone comes in and tells me that they want to train to be the first person on Mars, we’re going to dig into how astronauts train and develop a plan for working toward that goal.”
Training for Mars may seem extreme, but Kyle and his team don’t judge people’s ambitions, they facilitate the work necessary to reach them.
Finding a place
That includes Miranda O’Bryan, Miss South Dakota 2023, who is training for her chance to become Miss America 2024 in January. Miranda has been training at the Sports Performance Institute since 2021. “I graduated from college and started my career during the pandemic, and I needed to find a space where I felt comfortable. I tried a few different gyms and there was nothing wrong with them, but I hadn’t found a place that was the right fit,” she said. “When I found the Sports Performance Institute, I figured I would give it a try with the one-week free trial, and I have been training there ever since.”
It can be challenging for people to find the right gym, no matter what their fitness level and goals. Miranda liked everything that the Sports Performance Institute provided, like weight lifting, the equipment in the cardio room and yoga classes. “More importantly, the people there made it such a welcoming environment. It didn’t matter where I was starting or where I was on my health and fitness journey, they were excited that I was there.”
“Unfortunately, a lot of people have had some negative experiences at a gym, or just haven’t found one where they feel at home. We’re competitive people — that’s why we do what we do, and it’s important to us that we motivate our clients to do their best,” said Kyle. “That doesn’t mean acting like a drill sergeant all the time. We find out what works best for each individual, but the rule of thumb is that everyone is welcome here.”
A different kind of training
When Miranda was training for the Miss South Dakota competition, she found that she had some needs that are a little different than what you might see from traditional gym-goers.
“I was really thankful that they allowed me to use the studio space when it wasn't being used for classes. I've practiced singing, which is my talent, in the studio space. I've also used that space to practice walking in my evening gown,” Miranda said. It may seem like an odd request, but it was important that she have a flat open space with mirrors, and having access to the sound system didn’t hurt either.
“We don’t see a lot of our clients in the facility practicing walking in evening gowns, so it was a little unusual in that respect,” said Kyle. “But if we had a bodybuilder who wanted to practice poses in front of the mirror wall, no one would think twice. No matter what competition people are training for, we’re here to help them succeed. It doesn’t matter if they’re roping, swinging bats, running down fields or walking confidently in an evening gown.”
“I showed up with a bag of dresses in my arms and the trainers were absolutely committed to helping me prepare, and I just thought it was so funny walking around the gym in an evening gown,” she added.
Get to know Miranda
Miranda is a South Dakota girl through and through — she grew up in Martin, graduated from SDSU in 2020, and now resides in Rapid City where she has worked for KOTA Territory News and KEVN Black Hills FOX. She says the three most important things in her life are her friends, her family and her cat.
Miranda’s initiative for her year as Miss South Dakota is literacy based — she wants to get as many people reading as possible. As part of this, she hosts a podcast called Page Turners, where she speaks with authors, literacy advocates and people from across the country on unique reading journeys.
The next big thing
As the new year approaches, so too does the Miss America Competition, and Miranda is committed to being as prepared as
possible. That means keeping up with her physical training. “When I started competing, we still had swimsuit competitions, but over the years that has changed, and now we have a health and fitness category,” Miranda explained. “The idea is that you’re looking at overall fitness. You need to be physically fit to sustain this yearlong opportunity, but also you need to be mentally and emotionally healthy as well. That's been really important for me to share with people. No matter what you do, or what you're passionate about, you need to be healthy in all areas of life.”
Recognizing the importance of health and fitness has led Miranda to become an ambassador of the Sports Performance Institute. “I approached them and we had a great conversation about how being Miss South Dakota and preparing for Miss America is, in a way, similar to preparing for any competition,” she said. “Not the same, because I’m definitely not a professional athlete, but as an ambassador, I can help share how important health and fitness is for everyone.”
Kyle is happy that Miranda is able to reach an audience of potential clients that may not realize everything that exos has to offer. “We’re great at connecting with the competitive athletes, but people who aren’t in that world may not be aware that we’re here for them too,” he said. “The same things we focus on with our pro athletes — mindset, movement, nutrition and recovery — will help anyone achieve their goals, no matter what they are.”
“I can’t say I’ve ever watched a Miss America competition,” Kyle added with a laugh. “But we’ll be cheering for Miranda in January, that’s for sure — she’s one of us. She’s a contender.”
Listen to Miranda’s podcast, Page Turners, here.
Written by Wade Ellett
Photos by Bob Slocum
In our inaugural issue, we introduced you to Carter Berlin (One Tough Ten Year Old, Spring 2021), a young man who lives with a rare chronic autoimmune disorder. Three years later, Carter is still a regular visitor to Monument Health for infusion treatments.
What’s changed the most since he became a regular visitor to the Pediatric Unit is Carter himself. He has grown since being diagnosed at age 4 into a good-natured and humorous teenager who enjoys pepperoni pizza and roller coasters.
At 13, Carter is in a typical phase of discovery. He loves video games and horror movies, is getting interested in music and has been trying new sports like basketball and soccer. He bowled on a team with his older brother Mason, 15, in the Special Olympics state tournament recently.
“I like playing sports because you get to socialize and compete,” Carter said. “That’s what makes me feel excited; just getting to do fun things that make me feel like a normal kid.”
A diagnosis of Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) was the beginning of a new journey for Carter and his parents, Heather and Ryan, in treating and managing the condition. At 4 years old, Carter began to stumble and fall frequently. That’s when his parents first became concerned. As things progressed he lost the use of his limbs and large motor functions at times. Carter’s CIDP causes his body to attack his myelin sheaths, the fatty coverings that protect his nerves. Carter was first diagnosed and given Immunoglobulin (IVIg) therapy treatment at Mayo Clinic.
At Monument Health, the Rapid City Hospital team works closely with Carter’s care team at Mayo Clinic to carry out his plan of care closer to home. He comes in several times per month to receive infusions through an IV port in his chest. It’s a long 6-hour day when taking infusions, but he breaks it up by gaming and reading. Physically, Carter has ups and downs dealing with CIDP. Some days he has more energy and endurance than others. He is enrolled in physical and occupational therapy to help him stay active.
“I would describe myself as someone who wants to make everyone laugh and tries his best to be nice.”
- Carter Berlin
Carter shared that he has recently been diagnosed with autism, something he says has informed his perspective about his CIDP, adolescence and life in general.
“It makes me feel like what I’m going through is more normal, and I understand why I feel awkward sometimes,” he said.
Carter goes to middle school half days and enjoys reading and math. He says he enjoys the way math gets his brain working in problem-solving mode. His dad says he is proud of Carter for learning to live day by day and discovering things he is passionate about.
“Carter is a trooper. He’s been through a lot,” Ryan said. “What he can do any day just depends on how he’s feeling, but he pushes himself really hard to get through the day and to be able to do the things he enjoys.”
He has been billed in these pages as a tough guy, and rightly so, but Carter just wants to make you smile.
“I would describe myself as someone who wants to make everyone laugh and tries his best to be nice.”
Story and Photos by Bob Slocum
Read our origal coverage of Carter's story here.
Leaving your community better than you found it — there’s something inside of us that flourishes when we have a hand in that. If you’re looking for a heightened feeling of gratitude and a greater sense of purpose, improving your community is a great place to start. It’s even more powerful when you’re able to see the effects of those changes. Kelly Howie and his team believe that everyone should make a point to discover that kind of special touchpoint in their community.
Kelly owns RE/MAX Advantage in Rapid City. He and the two broker associates on his team, Ashley and Kylie, discovered a cause they’re passionate about in 2018, when they were presented with an opportunity to make an ongoing impact in the Black Hills.
Upon the completion of every real estate transaction that the team is a part of — whether buying or selling — a donation is made to benefit the Children’s Miracle Network (CMN) through the Monument Health Foundation.
Ashley Reed loves sharing the joy of generosity with her clients. “I have always felt that when you give to your community, your community gives back to you,” she said. “If you lose a sense of community, it just makes life a lot harder. So making sure that we have that sense of community and our clients have it too, has been amazing.”
Kelly and his team have earned the honor of being called Miracle Agents because of their dedication to the Monument Health Foundation and the Children’s Miracle Network. “By achieving the distinction of Miracle Agent, this team demonstrates their level of commitment to the health and wellness of the communities and families they serve,” said Shawn Powers, CFRE, Development Coordinator of the Children’s Miracle Network at the Monument Health Foundation. “Our youngest patients are very fortunate to have such strong Children’s Miracle Network champions in the Kelly Howie Team at RE/MAX Advantage.”
Personal ties
Kylie McMullin explained that making these donations in their clients’ name is usually appreciated more than other gifts that real estate agents typically send their clients. “We always joke about sending things that people will never use or just shove into the corner. But because almost everyone has had a friend or family member who has been personally involved with the Children’s Miracle Network, we thought that investing in CMN would be something that would speak to every one of our clients.”
Kelly and his team started the process of determining the best way to give back to the community by looking for personal ties to organizations and causes. “I do have a personal connection to the Children’s Miracle Network,” Kelly said. “My son was in the NICU for a period of time when he was born, and seeing the staff work — they were just tireless; they’re amazing in that section of the hospital. And beyond that, what it does for the families of the children who are there — the access that it provides, the comfort that it gives to the kids — it’s incredible.”
Kelly and his team encourage others to look for those same sorts of personal ties in the community to know where best to invest and serve. “If you’re looking for some way to invest in your community, consider the Pediatric Unit at Monument Health. It has had a huge impact on us,” Kelly said. “Your donations stay local, and you know your gift is going to help make sure every child in our community has a chance at the best care possible.”
Written by Stephen Simpson
Photos by Bob Slocum
Jason Olivencia is a car guy. The 12-year enlisted Air Force Technical Sergeant has a set of wheels to match his passion: a custom 2005 red and yellow Ford Mustang Joey Logano Hot Wheels replica. His car’s build has many features you’d expect from a car show-worthy ride: custom intake, exhaust, racing seats and endless upgrades.
When Jason’s Ford rumbled into the Monument Health Rapid City Hospital parking lot in October, it was filled with a donation to the pediatrics unit that represents his other hobby: collecting Hot Wheels.
Jason and his Mustang are aligned with Driven Dreams, an organization that holds an annual event to donate Hot Wheels to hospitals and other charities or organizations that accept donations for children.
This was the third annual national Diecast Day of Giving and the second time Jason has brought toys for Monument Health’s youngest patients. He brought 1,000 cars the first year and even more this fall.
Jason gave first dibs from numerous boxes full of sealed Hot Wheels to some patients in the pediatrics unit, taking some time to share videos of his car and wishing the patients and their families well.
“We really had some happy kids, and we will continue to get smiles over the next year as we hand them out,” said Amanda Horsley, Manager Nurse in the pediatrics unit. “Some of our kids go through some tough things here, and any little thing that can bring them happiness matters.”
The Texas native’s Hot Wheels collecting led him to start a YouTube channel called “Mustang Hunter Diecast,” and he has been part of an online collector’s community ever since. Multiple collectors joined together to ship Hot Wheels for a good cause the first year, and the event has grown from there, with organizers making donations in their local communities.
“The reward is just so great. Seeing the kids and their excitement reminds me of when I got my first car when I was a kid, and knowing that these will go to kids who are going through some hard times means a lot,” Jason said. “Knowing that one of them may spark an interest for some boy or girl to get into cars or Hot Wheels is awesome.”
Jason currently has 7,000 Hot Wheels in his “keeper” collection, most of them are different variations of Ford Mustangs.
“I love cool cars, and there are so many cars that I want when I see them. I'm like, ‘Man, I'd love to buy that,’” he said. “Hot Wheels comes out with every car you can think of, and that is my way of collecting them and checking those off my list.”
Story and Photos by Bob Slocum
From the outside looking in, it may look like Radiologic Technologist Robert Schroeder and his fellow caregivers have a straightforward job — creating high-quality X-ray images for physicians and their patients. But just like those X-ray images show, there’s a lot more under the surface. You just need the right tools to find what you’re looking for.
Some of the tools of the trade include curiosity, kindness and adaptability. “We never know what kind of a day we’re going to have until we leave,” explained Robert.
Perhaps it’s the ability and desire to learn and experience something new each day that has given Robert the drive to get to where he is. On July 1, 2023, Robert celebrated his 45-year anniversary working in medical imaging. An accomplishment like that doesn’t happen by chance.
“I’ve had various roles from staff technologist working nights to the Director of Medical Imaging Services. I still take X-rays, but I’m also certified to perform a CT scan,” said Robert, who is also the clinical preceptor for the Mitchell Technical College radiology students who rotate through Rapid City Clinic, Flormann Street.
“He’s an amazing teacher, he knows how to break things down for each individual so that they learn what they need to, which helps them become better caregivers,” said Julie Rueppel, Radiologic Technologist.
Julie has known and worked with Robert for 24 years. Both have seen their share of change, progress and growth, within their own roles and the industry as a whole. She’s adamant that through everything she’s seen, one thing has been consistent: Robert’s role as a mentor and teacher.
“He has taught me patience with our students — to slow down and make sure they understand what we’re trying to teach them. Because ultimately, we want the students to stay here and work at Monument Health.”
Not only is Robert inspiring new X-ray techs as they begin their careers, he’s also raising a member of the next generation of caregivers as well.
“My son is finishing his fellowship training at Mayo Clinic as a Neuroradiologist,” he said. “Next year he will move back home and work at Dakota Radiology. I'm getting close to retiring, but I told him I would wait until he gets started so perhaps he will be reading my images to care for his patients.”
Robert knows his career had an impact on the path his son chose. His ability to inspire others in this field means he can relax in his retirement, knowing there will be qualified and passionate caregivers to take over.
“I have been involved in the education of several technologists that are currently working for Monument Health.” Robert noted. “In fact, my current supervisor is actually a former student of mine.”
A Living History
“When I went through my training, I was taught how to hand-develop the X-ray images,” Robert said.
He’s witnessed, firsthand, the transition from film images to automatic processors and now to the digital imaging used today.
“The nice thing for a rad tech, and the patient, is that you can see the images right away. You don’t have to process them,” Robert explained. “You know right away if you need to repeat an image, so the patient doesn't have to wait around to know if the images are ok or if you need to retake something.”
The future’s so bright, you need to wear X-ray glasses
After 32 years working at Monument Health, Robert may be thinking about retirement, but there’s still more he wants to do. Specifically, he wants to continue inspiring, educating and training the students that will take his place.
“This is a very interesting career path. It’s what you make of it, and it's totally up to you if you want to advance in the profession, because there are plenty of opportunities,” Robert said. “I tell my students, ‘when you’re done and you take your boards for general radiology, don't stop progressing.’ I encourage them to take the CT Registry, or learn ultrasound, whatever interests them. I really encourage them to get another advanced specialty so they can move into additional roles.”
Robert, Julie and their team of X-ray techs are happy to tell you the importance of their roles, because at the end of the day, they know the most important thing is that they’re helping to care for patients.
“We do so much more than push a button on an X-ray device,” Julie said. “We really drive patient care by helping the patients feel comfortable in whatever exam we’re doing. We help them understand the process of taking the X-ray.”
Written by Stephany Chalberg
Photos by Bob Slocum
My Role
I am a Nurse Practitioner in general surgery in Spearfish. I work primarily with Andrew VanOsdol, M.D., in our accredited Bariatric Surgery Center of Excellence program. I am also fortunate to see patients for non-surgical weight loss using lifestyle changes and medications when needed.
My Goal
My goal is to provide excellent care to my community. I strive to establish a trusting relationship with each patient and want them to feel positive self worth. We collaborate to develop an individualized plan of care to improve nutrition, activity, energy and sleep while decreasing stress load. I aim to support each patient’s journey toward future goals of improved health.
My Passion
I am passionate about preventative health and setting an attainable example of a healthy lifestyle for future generations. I personally love running. It helps me to find daily mental, physical and emotional balance. I enjoy supporting others as they find and pursue their activities that bring about sustainable joy and long-term health.
Monument Health Spearfish Hospital is one of two Accredited Comprehensive Centers in the state designated by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, a national organization. This affirms that the hospital’s bariatric patients receive multidisciplinary medical care, which improves patient outcomes and long-term success.
My Role
First and foremost, I am a urologist who provides care to my patients. I am also the director of the Monument Health Robotics Program, which gives me the opportunity to collaborate with different specialties such as neurosurgery, general surgery and pulmonary medicine — which also use robotics during surgery.
My Goal
We are building a world-class group of robotic surgeons who are on the cutting edge of medicine — right here in the Black Hills. It's important to me that surgeries go well, the outcomes are good and we don't have a lot of readmissions or patients having to return for more unplanned care. To accomplish this goal, we are continuously building our robotics program to utilize the best equipment.
My Passion
I have a special interest in urological cancer and am passionate about providing great cancer care. I love collaborating with my colleagues in different specialties, such as medical oncology and radiation oncology, to give patients the best outcome they can get. We have a chance to cure a lot of diseases as surgeons and it makes me happy to be able to do that. One way we have ensured those high-quality outcomes is by expanding the technology with a single port robotics system.
Monument Health has the first single port robotic surgical arm in use in South Dakota. The single port reduces the number of incisions needed to perform surgery and is clinically proven to reduce post-procedure pain. The single port allows surgeons more versatility, allowing them to work in smaller areas or in areas with existing scar tissue.
In the early 1990s, two health care challenges were emerging in western South Dakota. First, the number of new family physicians practicing medicine in rural areas was not keeping up with demand. Second, the North Rapid City neighborhood was especially underserved.
Regional Health — now named Monument Health — devised a single solution that addressed both challenges. Its Family Medicine Residency Program provides new doctors with three years of residency training in family medicine. And the doctors work primarily at the Family Medicine Residency Clinic just off LaCrosse Street in the heart of North Rapid City.
The doctors work alongside experienced faculty physicians to hone their skills in obstetrics, pediatrics, emergency medicine, internal medicine, geriatrics and more. Most residents deliver more than 100 babies during their training, said Bobbie Schneller, D.O. She has been program director since 2017, and she too is a graduate of the program.
Each year the Family Medicine Residency Program accepts six new medical school graduates. Starting with the 2024 class, the program will expand to eight new doctors each year.
Community Closet
When Jennifer Callahan, M.D., was a second-year resident she saw first-hand how medicine alone is not always enough. She was treating an expectant mother at the Monument Health Family Medicine Residency Clinic in Rapid City. The patient was living on just $300 a month and couldn’t afford baby clothes. Dr. Callahan bought baby clothes, delivered the baby and continued ongoing treatment of mother and child.
“When her baby outgrew the clothes, she brought them back so another mother could use them,” recalled Dr. Callahan, who
is now on the Family Medicine Residency faculty. “It kind of snowballed from there.”
Today the Family Medicine Residency Program’s community closet features a wide range of clothing for patients and accepts donations from the public.
Family Medicine, Rural Health
Since the first graduation in 1997, nearly 150 doctors have completed the program. Sixty-seven stayed in South Dakota, and many have remained with or returned to Monument Health.
Sports Medicine Specialist Hollan Harper, D.O., is a good example. A native of Washington state, he received a Doctor of Osteopathy degree in Pennsylvania. He applied for residency at a number of family medicine programs. He was accepted by Monument Health.
“I was completely unfamiliar with Rapid City before coming here for my Family Medicine training,” he said. “For three years I had the wonderful opportunity to train with some amazing individuals, and I became close friends with many of them. It was primarily friendships my family and I made and the community atmosphere that made us consider staying here in Rapid City.”
Monument Health offered Dr. Harper a sports medicine position at the new Monument Health Orthopedic and Specialty Hospital. After completing a fellowship in Sports Medicine in Texas, he returned to Rapid City in 2020.
The medical clinic provides a range of services for patients of all ages and income levels. The list includes obstetrics and newborn care, minor surgical and dermatology procedures, onsite laboratory and X-ray services, well-child visits, women’s care, vascular screenings, Medicare wellness visits and nursing home patient visits.
Nutrition Training
For Family Medicine residents, nutrition is part of the training. As an exercise, each resident must create a nutritious one-week meal plan for a hypothetical family of four — including a father with diabetes. And they have a budget of $150, the amount a family would receive in Supplemental Nutrition Assistance Program benefits. “It's very easy to say, ‘Well you need more fish, chicken and fresh fruit in your diet,’ but when they realize how little these patients have and how much these foods cost, it changes how they approach their patients,” said Bobbie Schneller, D.O., Director of the Family Medicine Residency.
Food Pantry
In low-income or rural communities, patients don’t always have access to fresh, healthy foods. They often end up subsisting on fast food or convenience store foods, both of which are high in fats and carbohydrates.
“We can give our patients all the medicine in the world and have these great health care plans. But if they can't afford it, it doesn't matter. They don't get healthy,” Dr. Schneller said. “And so we're trying to figure out how we can mitigate some of those circumstances for our patients.”
The program’s food pantry distributes about 2,000 pounds of food per month to 45 patients and their families, said Mary Beth McLellan, RN, who has been involved in the pantry since it began. In addition to food, the clinic provides cooking equipment that has been donated by community members.
Services provided at the Family Medicine Residency Clinic:
• Annual exams
• Diabetic retinal screenings
• Laboratory services
• Medical imaging services
• Medicare wellness visits
• Minor surgical procedures,
including vasectomies
• Newborn care and
well-child visits
• Nursing home patient visits
• Obstetrics
• Primary care for the
whole family
• Vascular screenings
• Women's care
Accepts most major insurance plans
including Medicaid and Medicare.
Written by Dan Daly
Photos by Bob Slocum
Hang around a tattoo shop for a while and you’ll see all kinds of art pass through the door. Rose tattoos with a loved one’s name, cosmic planetscapes, geometric patterns and meaningful dates. Of course, every shop is different, and at Emma Madsen’s studio, Duende Ink, what you’ll find are graceful fine lines creating elegant designs.
“That’s what I’m most known for,” Emma said. “I do try to incorporate a wide variety of styles, and try to blend my style with what my clients want, but I’m usually known for the fine lines.”
That may be Emma’s signature style, but there's another technique that she’s grown passionate about — microblading. From a technical perspective, this differs from traditional tattooing, which uses a needle to inject the ink into the dermis, the second layer of the skin. Microblading uses a small blade to make fine, hairlike cuts in the top layer of skin, called the epidermis. “After the cuts are made, you gently stretch the skin and then add the pigment,” Emma explained. “It’s considered cosmetic tattooing, and is most commonly used to create or enhance the appearance of eyebrows.”
When it comes to tattooing, Emma is largely self-taught, but cosmetic tattooing like permanent makeup and microblading are specialized skills — after graduating esthetician school at the beginning of the year, she traveled to California for training to master them. Since then, microblading has become popular among her clients, and it's a service that Emma has decided to offer to cancer patients free of charge.
“I had one of my clients here and she works at Monument Health, and I brought up the idea of doing free eyebrows for cancer patients. She was excited and put me in touch with the people at the Cancer Care Institute,” Emma explained. “I told them what I wanted to do — the initial idea was to actually go to the hospital and do the microblading there, but we weren’t able to do that yet. Instead, we started with gift cards for free microblading.”
Meet Tina
“I had breast cancer in 2012, localized on the right side,” said Tina Kettner, one of Emma’s clients. Because of a family history, she opted for a preventative mastectomy paired with chemotherapy and has been cancer free since then. “In the process, I hardly lost any hair, but for some reason I lost my eyebrows and eyelashes.”
Tina was one of Emma’s first microblading clients, and the effects have stretched far beyond simple cosmetics. “There are so many challenges when you’re going through cancer, and you can lose your identity with these changes inside and outside of you,” Tina said. “It made me feel more confident in myself when she did it — it made me feel like a woman again.”
“I think it’s incredible what Emma is doing, giving back to the community and cancer survivors. There are so many people affected by cancer, and this may seem like a minor thing, but it’s so impactful to us,” she added.
Because chemotherapy weakens patients’ immune systems, they need to wait six weeks after their final treatment to get the procedure done, and then get their physician’s approval. Emma is excited to continue to help cancer survivors feel like themselves again and hopes that soon she can work with the Monument Health Cancer Care Institute to provide microblading in the facility’s salon.
Caring for her community
Emma is aware of how much cancer can affect a family and a community. “I had a cousin who was diagnosed with colon cancer in 2021. She passed away at the age of 27. A family friend passed away last year from cervical cancer. Everyone knows someone who has been touched by cancer,” she said. Emma credits the experience of growing up in the small town of New Underwood for helping her see how connected people are. When you lose just a few people in a small town, she explained, you see how significant the impact is on the whole community.
“People care about others in their community, and when someone is affected by cancer, we want to help,” Emma said. “This is something I can do. It’s easy for me, but it can be life changing for them — that makes it worthwhile.”
Tina added, “What she’s doing, it can give you hope. It’s a piece of the puzzle moving forward after you’ve overcome cancer. You’re able to look in the mirror and think, ‘this is great, here I am again.’ I can’t say how
grateful I am for how Emma has helped me feel like myself again.”
Written by Wade Ellett
Photos by Bob Slocum
When eight-year-old Rayne Rucker entered the Central States Fair on August 23 for Monument Health’s Special Rodeo, she knew just what she wanted to do: everything!
By the time Rayne was seated in the saddle of a practice bucking bull, she was no greenhorn. She had already ridden a horse, had her face painted, run a barrel race and cuddled with therapy animals. The one constant as she enjoyed the different stations was an exuberant smile and frequent gleeful giggles.
Waving one hand in the air and hanging onto the saddle with the other, Rayne beamed at her mother, Miranda. Rayne is a lot like any other third-grader, she just gets around differently. When she needed a hand or a boost she received one, but nothing was stopping her from getting all over the arena and enjoying the event to the fullest.
At Special Rodeo, no one is defined by their limitations. Participants are rodeo cowboys and cowgirls first and foremost. That’s been the mission behind the event since the start: rodeo is for everyone. Each person has a place here and everyone is a champion.
“It was so much fun,” Rayne exclaimed. “My favorite part was getting to pet the duck, named Cheese. My second-favorite part was the horses; actually all the animals!” Miranda said it is not always easy for Rayne growing up different from other kids. Special Rodeo is meant to provide an inclusive, supportive environment where all feel free to enjoy new experiences.
“Sometimes other kids are a bit standoffish because of her physical differences, but once they get to know her, they do really well with her,” Miranda said. “She’s not different, she’s unique.”
About 100 participants with special needs – aged 5 to 80 – and 170 volunteers converged on the James Kjerstad Event Center, where western activities and fun galore awaited them. Participants were partnered with a “rodeo buddy” who showed them the different stations and cheered them on.
The free event offered horseback rides on certified therapy horses from SunCatcher Therapeutic Riding Academy, stick horse barrel races, roping, a goat ribbon pull, miniature horses, face painting and other therapy animals to interact with. A sensory area was provided for contestants when they needed a break. Each participant received a t-shirt, a trophy belt buckle and lunch. The Special Rodeo is also held in January during the Black Hills Stock Show, in partnership with Rodeo Rapid City.
The success of the Special Rodeo hinges on a sincere mission of inclusion and respect. Among the key organizers are neighbors from the local farm and ranch community who create an authentic western atmosphere, where differences are not only accepted but embraced. Participants have an opportunity to experience the thrill of rodeo and a connection with animals that brings a distinct expression of fulfillment to faces throughout the arena. Kami Peri brought her daughter, Sayler, to Special Rodeo in the past. Although Sayler, 5, isn’t very verbal, she told her mother just how much fun she was having with a mile-wide smile.
“Seeing her shine in her moment and feel like a million bucks just made my heart explode,” Kami said. “We really loved that everything was geared towards her.”
Rhonda Fuhrer, Supervisor of Business Operations at Monument Health Belle Fourche Clinic, got the event started by bringing the idea to Anna Whetham, Community Relations Specialist at Monument Health. She had been involved in similar events and thought Monument Health would make an excellent partner for this rodeo. In just a short time, she said, interest in the event from participants and volunteers alike has exploded.
“It is only going to continue to grow,” Fuhrer said. “You can’t take part in this and not feel good about the impact it makes.”
Rhonda understands how meaningful and therapeutic these kinds of activities and access to animals can be. She lives on a small acreage and is mother to a 23-year-old special needs daughter, Morgan. Morgan rides horses at home with the help of a custom saddle, and her family has long made modifications so that Morgan can be involved.
“It’s humbling. It can take some effort, but she’s made us better people,” she said.
The western spirit shines through when participants and volunteers meet in the arena, pairing together friends new and old. For a growing number of participants and volunteers, returning to the event each time is a chance to reconnect with their rodeo buddies. As they circulate through the stations, accommodations are made and encouragement given with the goal of giving each guest a great experience.
“Rodeo is for everybody, and this is a great event to show it,” said Glen Lammers, Black Hills State University Rodeo Coach. “I thought Monument Health did a great job with the events. 
The bull and the roping steers are equipment we would use to train with, so it’s the real deal.” Lammers has brought members of his team multiple times to assist as rodeo buddies.
“What stands out is the enthusiasm and infectious positivity they bring,” Lammers said of the rodeo participants. “You can’t help but smile with them. We get more out of it than they do, probably.”
Amy Morrill, Nurse Clinician for Rapid City Hospital Pediatrics Unit, has helped volunteer along with her fellow pediatric nurses at previous events.
“It is an absolute blast,” Morrill said. “For the pediatrics team, kids are our jam. When we get to bring joy to kids outside the hospital, it’s like icing on the cake.”
Abounding support for the event proves just how much it has resonated with the intersecting communities which cooperate to make it possible. For the participants it is a chance to be celebrated, to feel included and empowered, and to experience the sport of rodeo in a way that is tailored just for them.
“We’re all unique but we can experience the same joy,” Fuhrer said.
“It is only going to continue to grow. You can’t take part in this and not feel good about the impact it makes.”
RHONDA FUHRER
Supervisor of Business Operations, Monument Health Belle Fourche Clinic
Story and photos by Bob Slocum
In 1999, Britney Spears sang the words, “My loneliness is killing me…” Those lyrics weren’t meant to be taken literally, but Britney was ahead of her time — new evidence indicates that loneliness has an incredibly detrimental effect on our health.
But you don’t have to just take Britney’s word for it. Last spring, the Surgeon General of the United States, Vivek Hallegere Murthy, released a bold statement: loneliness is a public health epidemic. In the 85-page document that accompanied this declaration, the surgeon general and his team cited research that made the eye-catching claim that chronic loneliness has the equivalent outcome on an individual's mortality as smoking 15 cigarettes a day.
It’s easy to understand how factors like obesity, smoking and contagious diseases are connected to matters of public health — their impacts are observable. Mental health ailments, on the other hand, tend to work less visibly and in more incremental ways. Smoking clearly causes emphysema, but can moods, feelings — whatever you’d like to label them — like loneliness really take years off our lives?
Strong enough to ask for help
Joy Mueller, M.D., is a Family Medicine Physician at Monument Health Sturgis Clinic. For the last five years, she’s helped the people of Sturgis and other Northern Hills communities live healthier lives. Dr. Mueller has a deep understanding of how mental health can’t be ignored if individuals want to get the most out of their health. So, when she read that the surgeon general compared loneliness to smoking, she wasn’t surprised.
“What the surgeon general said is really important because he called out that our health is more than just our labs and our vitals,” Dr. Mueller said. “He really brought attention to the idea that there's so much more to ourselves — that the support and the people around us and how we choose to interact or not to interact with people around us is an important part of our health.”
Dr. Mueller said that she encourages her patients to not neglect their mental well-being, and that receiving support isn’t a luxury; it’s a critical component of their overall health. But, she said that this view of mental health as a necessity often clashes with some of her patients’ lifestyles. “In South Dakota most of my patients are self-reliant, hard-working, strong people. So asking for help or support can be challenging.”
Dr. Mueller pointed to her aging patients or patients who receive serious diagnoses like cancer as prime examples of individuals who have a strong potential to isolate because they don’t want to burden their loved ones. “We have a lot of conversations like this: ‘Your son, or your daughter or that nice lady who brought you last time seemed to really enjoy being here with you. Why don't we give her a call?’”
These sorts of conversations play a serious role in the overall health of a person — if someone is missing doctor’s appointments or can’t make it to the pharmacy or grocery store, their overall well-being is going to take a hit. And research has shown that isolation, as the surgeon general pointed out, can cause the systems of the body to deteriorate in measurable ways. That’s why Monument Health has invested in the mental health needs of their patients with the presence of caregivers like McKenzie Grim.
A non-negotiable
McKenzie Grim, CSW-PIP, is a Licensed Clinical Social Worker who practices alongside Dr. Mueller at the Sturgis Clinic. “People will often hear the term social work and assume case management or social services, but once you reach the master’s level, the focus is mostly psychotherapy, and that’s primarily my job description at the clinic,” she said.
McKenzie helps patients see a complete picture of wellness — that regular social interaction isn’t a nicety; it’s as important to our health as eating healthy or exercising. “Your physical and mental well-being is the core of your everyday life,” she said. “It is non-negotiable. Are you surviving, or are you living?”
McKenzie has said that loneliness doesn’t discriminate, and that anyone has the potential to suffer from isolation — including families. “Family time is so important, but being in a dual income household is more common than not,” McKenzie explained. “Daily schedules really help a family maintain continuity for everyone. Twenty minutes a day of quality time with your family has the potential to increase your overall well-being.”
Like Dr. Mueller, McKenzie wasn’t surprised when the surgeon general sounded the alarm about loneliness in the U.S. “I don't think the topic of loneliness is new, but COVID-19 ripped off the Band-Aid,” she said. “The surgeon general’s office has categorized it as an epidemic, but it has been around for at least the last five years. It can cause issues with blood pressure and BMI, as well as your mental health. However, all of these things are manageable.”
Major diagnoses like cancer usually receive an automatic referral to mental health professionals like McKenzie. “Usually the first time I meet with someone, I just let them know that I’m here for them; that I’m not going to force myself on them or judge them — that I’m just a part of their toolkit.” A complete picture of wellness must include an honest look at mental health. As McKenzie pointed out, it’s non-negotiable.
Sometimes, finding opportunities to socialize can be difficult, especially in a rural setting. McKenzie has a tip on building self-confidence and combating loneliness in rural South Dakota: “Small towns are really trying to encourage more community gatherings. Throughout the Black Hills we see opportunities to socialize are out there; I encourage everyone to search them out.”
Dr. Mueller said of McKenzie, “She’s wonderful at her job, and we are so fortunate to have her in our community. I really think that’s one of the things that the surgeon general is getting at. How can we provide more mental health support for people?” Both McKenzie and Dr. Mueller appreciate that Monument Health has invested in treating both the physical and mental health of patients by having social workers, counselors and other mental health professionals readily available to patients.
Written by Stephen Simpson
For Lito and Lucita Casilang and their daughter Sandra Gruenig, Rapid City is very different from their native Philippines 7,500 miles away. The food, the culture, the weather — especially the weather — are different.
But what is not different is that hospital patients need to receive health care with skill and compassion. The family’s hard work and attention to detail has attracted the attention of patients and staff.
All three family members work at Monument Health Rapid City Hospital. Sandra is a Registered Nurse in the Float Pool. Lito is a Nurse Aide in the
Progressive Care Unit. Lucita is a Nurse Aide in the Inpatient Oncology Unit.
In August 2021, Sandra received the hospital’s DAISY Award for RNs who go above and beyond in patient care. In January 2023, Lito received the TULIP Award honoring support staff who make a difference in the lives of patients and families. And Lucita received employee of the month honors in her oncology unit.
Sandra believes that the family’s awards could be due in part to the Philippines’ culture, which emphasizes extended family and care for others.
“I know when a person loves his job. Lito goes out of his way to clean and to ensure everything that needs to be done is taken care of.”
- Tulip Award nominator
“We do not have nursing homes and assisted living in the Philippines. We take care of our families at home,” Sandra said. “And when you say family in the Philippines, you don’t mean just your mom and your dad. It’s your aunts, your nieces, your cousins.”
Marriage brought Sandra to Rapid City in 2015. Two years later, she began work as a nurse aide while attending nursing school. She graduated in 2020 and became an RN. Her class was the first group of new nurses to start their careers during the COVID-19 pandemic.
After achieving citizenship, Sandra filed a petition to bring her parents to the United States. Neither had a health care background. Lucita had a small business in the Philippines, and Lito, who studied law in the Philippines, was working as a security officer and sometimes bodyguard at the Saudi Arabian Embassy in Amman, Jordan.
“When I came here, I was thinking of a job maybe in security or cleaning. I did not think I would be employed as a nurse aide,” Lito said. He admits he was a little intimidated by the idea of patient care at first. “As a security officer or a bodyguard, for example, you will just look around for a suspicious person. And that's it,” he said. “As a nurse aide, you will go into the room and take care of the patient.”
One of the patients who nominated Lito for the TULIP Award wrote: “I know when a person loves his job. Lito goes out of his way to clean and to ensure everything that needs to be done is taken care of.”
Lucita, who started work as a nurse aide in July 2022, said she also loves her job, even though it can be difficult working in inpatient oncology. Some of the hospital’s sickest patients are treated there. And she still is trying to adjust to South Dakota’s winters.
Two more members of the Casilang family, Sandra’s brother and sister, are still in the Philippines. Lucita said they hope to bring them to the United States as well.
Written by Dan Daly
Photos by Bob Slocum
For most people, a hospital stay isn’t a great time in their life. It can be scary and uncomfortable, often coming as an unpleasant surprise. However, there are things that can make it a little better, including hearing from loved ones.
Just ask Mahra Wick and Isaac Thompson.
Mahra and Isaac are a fun couple — they just seem to go together, like peanut butter and jelly. On break from the University of Wisconsin at Stevens Point, the two decided to take a vacation together, visiting three National Parks — Rocky Mountain, Grand Tetons and Yellowstone. They bring out good humor in one another, and conversations tend to be cheerful when they’re in the room. That even includes their hospital rooms after a driver going 80 miles per hour in the wrong lane collided head on with their vehicle.
They both needed serious medical attention, especially Mahra, and Monument Health was able to provide that care. But stepping into their hospital rooms, you’d notice that they received more than clinical care — their walls were plastered with printed cards, part of an E-card program provided by Monument Health.
“At first, I didn’t even know this existed, and then we both started to get cards from my family and his family,” said Mahra. “People I’ve never met before sent me prayers and blessings on the cards. Some brought me to tears and others gave me a couple of laughs and smiles.”
“It has been mind-blowing. The cards really brightened my time here,” she added.
A silver lining
“The E-cards are something that came out of COVID-19,” said Pete McQuiston, Director of Food and Nutrition Services for Monument Health. “Everyone was coming together and trying to find ways to help our patients, and one thing that came up a lot is that patients couldn’t have visitors.”
Pete explained that developing the E-card program was an effort that involved a lot of stakeholders across the organization — IT who built out the process, Public Relations and Marketing who designed the cards and Food and Nutrition who delivered the cards with the patients’ meals.
The COVID-19 pandemic has passed, but the E-cards have stuck around. “It still gives friends and family members a way to stay in contact with their loved ones if they can’t come visit in person or live far away,” said Pete.
Since the pandemic ended, Guest Services at Rapid City Hospital has taken on the task of delivering cards to patients. For Judi O’Connell, the Manager of Guest Services, this is a highlight of her role. “It’s so awesome getting to take the cards to people,” she said. “You can see how it brightens their day.” Judi encourages as many folks as possible to send E-cards to patients that they know. “Sometimes people can’t come and visit as often as they’d like, or they just want a way to send someone a smile, and the E-cards are the perfect way to do that.”
Judi O'Connell
Manager of Guest Services
“There is something a little bittersweet about my role — I’m always sorry that anyone needs to be in the hospital, but I’m grateful to do everything that we can to make their stay a little more pleasant. Whether that’s delivering an E-card or helping them be more comfortable. That’s what Guest Services is all about. We may not be able to help heal anyone in a clinical sense, but I believe we can help them feel better.”
Keeping in touch
Because Isaac and Mahra were on vacation, no one was nearby to visit them right away. To make matters worse, both their phones were lost in the accident, so friends and family members couldn’t reach out via text or social media. Instead, the two were flooded with E-cards.
“It completely made our day when we’d see Judi come in with a folder,” Isaac said with a chuckle. “She’d come in waving it, saying, ‘You got more!’ and it was a lot of fun. It was awesome, and really powerful. It made us both feel better knowing that people were thinking of us.”
Before long, they were locked in a fun-spirited competition — who would receive the most E-cards? “A couple of Isaac’s uncles started to send multiple cards with jokes on them,” Mahra said, “And my brother sent one that said, ‘I hear there’s a competition now, so tear it up!’”
Jennifer H asvold, M.D.
asvold, M.D.
Hospitalist
“Being hospitalized for an acute illness is an almost universally stressful experience. For many of our patients, staying connected to their loved ones makes all the difference. It’s easy to feel a sense of despair and isolation during a hospital stay, and I really see patients light up when they talk about the important people in their life. We serve a very large geographic area and many of our patients have friends and family who are thinking of them but are unable to visit in person. Cards and E-cards are a wonderful way to show patients that they are cared for. Healing is about much more than medicine — even small reminders to stay positive can make a huge impact.”
A little piece of kindness
Not everyone gets into a competition over who gets the most E-cards, but many people are happy to receive them during their stay at Monument Health. “So many patients are excited to share the messages they receive, and I’m always happy when they tell me what people have written. It’s a little piece of kindness that we get to share.” Judi said. “One woman received an E-card each day from her daughter, and it was so meaningful to her. We’ve had patients receive cards from across the country, and even from all over the world. It’s incredible.”
Pete echoed this sentiment and said, “We don’t have the same restrictions on visitors that initially led to the creation of this program, but it’s still a way to stay in contact. It’s great that this is so well used by the community and even by people from far away.”
“Morale is important, and I think there’s even an argument to be made about boosting patient satisfaction, improving recovery times and maybe even improving length of stay times,” Pete added.
Isaac and Mahra agreed. “Just getting these cards from everyone, it made us feel a whole lot better about our situation. It’s powerful,” said Isaac.
“I wish this was a common thing. I wish that everyone got these because they really did brighten our time in the hospital and made us forget for a few moments that we got in this accident,” added Mahra. “We got to hear from so many different people. I know Isaac got a bunch of cards from my family members who he’s never met before, and I got them from his family members who I’ve never met before either. It’s like we got to interact and connect with these people. Even though it was unfortunate circumstances, it was really a great experience.”
Written by Wade Ellett
Photos by Bob Slocum
People love their pets, and with good reason — research indicates that pets can improve our lives. Some studies have shown that our furry friends can decrease stress, improve mental health and help children with emotional and social skills. Not to mention, being responsible for another living creature teaches kids the importance of responsibility.
Pets offer unconditional love and provide companionship to those who care for them. Choosing to have a family dog, a lovable lizard or even an army of sea monkeys may bring a little extra work, but the rewards are well worth it.
 Leslie Van Dyne, M.D., Trauma Surgeon
Leslie Van Dyne, M.D., Trauma Surgeon
Boomer is a rescue from Columbus, Ohio and he just celebrated his ninth birthday on Labor Day. About five years ago he lost both of his eyes after contracting a fungal infection. He gets around just fine though. The setback didn’t slow him down at all! He is thriving in South Dakota and loves getting out and about. Boomer is one lucky pup, when he isn’t begging for — and getting — treats, he loves lounging on his couch, going for walks and ear scratches. We were lucky enough to have Boomer join my now husband and I as the flower dog in our wedding. He is a natural in the spotlight and it made a magical day even more memorable.
Peter Ostler, M.D., Faculty Physician, Family Medicine Residency Clinic
I have six parrots: one Black-Capped Caique named Frida, one Sun Conure named Vincent, two Green-Cheeked Conures named Jacques and Rembrandt and two Lovebirds, Mater and Fezzik.
Frida is the largest and by far my favorite. Her black cap makes it look like she has a unibrow and reminds us of the famous painter she is named after. She loves to play and is a clown — because she loves to play, she also loves to explore different people. She is typically very gentle, but she has a very strong beak. If she is not happy with what you are doing she can take a wicked bite out of your finger.
gentle, but she has a very strong beak. If she is not happy with what you are doing she can take a wicked bite out of your finger.
Our Sun Conure is named after Vincent van Gogh because his colors are very similar to the colors used in the famous Sunflowers paintings. He loves my wife the most and will call out to her from our aviary in the morning as soon as he hears her voice. He is also very special to us because although he was bred in captivity, his species is endangered and there are an estimated 1,000-2,500 mature individuals left in the wild. They are very popular in captivity and as such there is a robust population left in the world.
Our Lutino Lovebird, Fezzik, is a strange one in that no matter the photo, his colors are so vibrant that it makes him look like he is photoshopped into the photo. His best friend is one of our Green-Cheeked conures named Jacques, and when out of their cages, they are never far apart.
 Ryan Gianatasio, M.D., Interventional Neurologist
Ryan Gianatasio, M.D., Interventional Neurologist
I love introducing people to Gus, our bearded dragon! This guy is about three years old but only joined our family a little over a year ago. We adopted him from another family who could no longer care for him.
Since then, he has gotten a lot bigger and has become just another member of the crew. He enjoys being with, on and around people and hanging out. For him, hanging out is just as comfortable on your shoulder as in his tank. His favorite foods are arugula, raspberries and mealworms. For the most part he’s pretty chill, but he definitely does not like baths in the sink.
Joy Falkenburg, M.D., Family Medicine
 I have many animals at my farm, from domestic to livestock. It was hard to pick which ones to highlight.
I have many animals at my farm, from domestic to livestock. It was hard to pick which ones to highlight.
The duck is Auggie. His mother abandoned the nest before he hatched and my daughter brought him in as he was breaking through the shell. She kept him under a light until he hatched and then he imprinted on us. We often use duck eggs in our baking as the slightly higher cholesterol levels make them nice for cooking.
The llamas are a mom and daughter pair that we received as a gift. They came to my farm after a patient was moving into town and couldn’t bring them in from her country farm. She wanted them to have a good life, and we benefit by having them protect our farm from coyotes and predators. We also have alpacas; they are smaller and produce fiber for gloves and hats.
Finally, this piglet belongs to my Mangalitsa pig, Natasha. She’s on her third set of piglets. My kids and I have farrowed the piglets together. We raise them for mmeat and they’re sold locally at The Shed at Dakota Greens-Custer Greenhouses and Nursery. When Natasha doesn’t produce enough milk, my husband helps bottle feed the piglets and even reads books to the mom when she’s heavily pregnant.
For parents, those opportunities are fleeting and bittersweet, as one day those moments will be gone.
But that’s not the case for the child care aides at the Monument Health Children’s Center. Here, each day is a new opportunity to rock a baby, watch a toddler take those first, uneasy steps and play hide-and-seek with spunky kids.
Samantha Chilstrom is a Child Care Aide at the Children’s Center. She works in the Tigger Room, surrounded by Pooh, Piglet and Roo, too. The youngest children of Monument Health’s physicians and caregivers spend their days in the infant to 3-year-old building under the loving and watchful eyes of child care aides.
As a growing employer in a growing community, Monument Health saw a need for more child care options. The Children’s Center was opened in 1981 as an affordable option to provide preschool and day care services to those working for Monument Health. Three buildings provide space for children of different ages, and both the day care and preschool are fully licensed.
“Our physicians and caregivers often make life and death decisions in their professional roles,” said Trina Allen, Vice President of Human Resources. “Having a safe, loving place for their children allows them to focus on delivering high-quality patient care — knowing we are providing love and care to their children.”
Samantha has been watching kids grow at the Children’s Center for seven years — and she loves what she does.
“Simply put, my role is to provide nurturing care to young children and services that support the needs of working parents,” said Samantha. “Each day I come to work with the goal of giving the best care I can to help these little minds grow into bright and caring young boys and girls.”
As a mom of three boys, Samantha said one of the unexpected perks for her is girl time.
“I always say, ‘my girls,’ and ‘my girl time is at work,’” said Samantha as she received an extra hug from Zoey. “I might not get to pick out the cute outfits, but I do love my girls — and the boys too. Really they’re all great!”
Inside the classroom, there can be joyful giggles, and nervous cries — especially when a little one is first dropped off in the morning. For the approximately 65 babies and toddlers at the Children’s Center, they don’t have to wait long or go far for a hug. There is always a friendly face with a warm smile close by for children needing comfort. Each of the 18 caregivers knows the children by name and has built trust to console even the biggest tears.
“Samantha is just an awesome caregiver who cares deeply for these kids,” said Shelly Godkin, Child Care Supervisor. “You can see she uses her whole heart to care for our kids. She absolutely loves her job and loves to be here and take care of the kids every day.”
Samantha and Shelly also agree it’s hard to have a bad day when you get so many hugs.
“If I’m feeling a little down, or just need something to cheer me up, I have the best job in the world. I get the best hugs and snuggles from these kids. It’s hard to have a bad day when you see how much love these kids have to offer,” said Samantha.
There are bittersweet moments: each year Samantha and her Tigger team say goodbye to their little friends who have taken up quite a bit of space in their teachers’ hearts. When the children turn three they move up to a new building, with new friends and new child care aides to love and learn alongside.
“It’s difficult to see them leave,” Samantha said. “You really build a strong bond with these kids. I try to visit them in the big kid building — it’s hard to say good-bye.” So instead of good-bye, it’s “TTFN! Ta-ta for now!
Written by Stephany Chalberg
Photos by Bob Slocum
The Heart and Vascular Institute (HVI) at Monument Health recently became one of the first hospitals in the U.S. to perform an innovative new procedure treating an uncommon form of heart arrhythmia.
The case required simultaneous collaboration between electrophysiology and cardiothoracic specialists to treat a patient suffering from inappropriate sinus tachycardia (IST), a disorder characterized by extreme racing of the heart for no known reason. The condition predominantly affects young women, many of whom are in otherwise good health. So it was for the patient who sought treatment at HVI and was referred to Ethan Levine, D.O., FHRS, one of HVI’s resident electrophysiologists.
“The patient had come to us with very troubling symptoms that had been going on for a while,” Dr. Levine said. “With IST the group of cells that govern heart rate are inappropriately overactive. It makes it so everything you do feels like running a marathon.”
As alarming as the symptoms are, IST can be challenging to diagnose in the first place. Those with the disorder may experience palpitations, general weakness, tremors and exercise intolerance.
“It's a very tough problem for a few reasons. One is that it's very often misdiagnosed as anxiety or something else,” Dr. Levine said. “So it can be very frustrating for the patients. And then you can also imagine that if you're not feeling well, you stop doing everything. Then you lose your quality of life and you get de-conditioned and depressed. All these things compound each other.”
Dr. Levine was aware of an ongoing study overseas that showed promise. It involved a tag-team approach with an electrophysiologist and a cardiothoracic surgeon, who would work together on the hybrid thoracoscopic ablation. He reached out to Charan Mungara, M.D., a Cardiothoracic Surgeon at HVI, and asked if he would like to collaborate on the procedure.
“This is an entirely new procedure for us, which works out because Dr. Mungara enjoys heart rhythm work and is very good at it,” Dr. Levine said.
Upon reviewing the study for the novel sinus node-sparing hybrid ablation procedure, Dr. Mungara was confident it could be done at Monument Health. The HVI team spoke with the AtriCure team running the study in Europe and Asia to coordinate a plan for the procedure. With HVI’s electrophysiology and cardiac surgery teams and the AtriCure team all on the same page, the procedure was scheduled.
“The company was great. They brought their whole team in from overseas and we got the case done, so I thought it was a win,” said Dr. Levine.
While HVI physicians have been performing convergent ablation procedures in which cardiovascular surgeons and electrophysiologists work in tandem to treat atrial fibrillation (AFib) in patients for some time, this procedure was unique. Both Drs. Mungara and Levine and their teams were in the operating room at the same time throughout the procedure, working to perform mapping and ablation simultaneously rather than 30 days apart.
“We’re one of the busiest atrial fibrillation places in the country, so the relationship that we have built with Dr. Mungara, that we built from so many convergent atrial fibrillation ablation cases, gave us confidence in his ability to do this.”
Using the relatively new Octaray multipolar mapping catheter device, of which Monument Health was the first hospital in South Dakota to have, Levine mapped the patient’s heart to create a three-dimensional electron atomic map, a computer model of the heart that plots the electrical signal in tens of thousands of places throughout the chambers of the heart.
“It’s kind of like a GPS, and after we get that model made we project it on a screen and then we can turn to the surgeons and say ‘that's where we want to be.’ It's like taking your EKG from 5,000 different spots.”
That is when Dr. Mungara and his team took the reins of the procedure. Mungara used catheters to reach the heart with a camera and his tools for performing acute actions to affect the sinus nerve. Once Mungara’s work was complete, Levine resumed mapping and recording rhythms, ensuring the desired result had been achieved.
“After he finished up, we went back in with our equipment and double checked that everything looked good and solid. If there were any gaps, anything that
could have been missed from the outside, we would have taken care of it from the inside. When we finished that, we removed all of our equipment, and Dr. Mungara removed his and the patient was off to recovery.”
In terms of acute recovery, the patient has had several incisions and they’ll be sore and in the hospital for a short stay, during which time the initial or junctional rhythm of the heart may still be abnormal. As the patient prepares to go home, wearable heart monitors are used to ensure normal rhythm is coming back.
Story and Photos by Bob Slocum
In our spring 2021 issue, we introduced you to Katie Young, a young woman who was celebrating her college graduation at a bowling alley when her heart stopped beating. You also got to know Amanda Gunter, the Registered Nurse who — coincidentally — was in the same bowling alley, and who saved Katie’s life.
Unbeknownst to Katie, she had a condition called Long QT syndrome (LQTS), which causes problems with the body’s electrical system that regulates heartbeat. Since our initial story about Katie came out, she met with a specialist at Mayo Clinic, who recommended a procedure called left cardiac sympathetic denervation. “This is where they go in and remove a portion of your left sympathetic nerve in your chest cavity,” Katie explained. This helps regulate heartbeat and minimizes the risk of future arrhythmias. “It’s not a cure. The LQTS will always be there, but they’ve reduced the problem, so it’s much less concerning.”
In addition to Katie’s good health, she has completed a tattoo apprenticeship and has spent the last two years tattooing at Good Dominion Tattoo Company in Rapid City. “I’ve been really busy but it’s great,” she said. “It’s crazy, you know? I get to see all sorts of different people every single day, and I’m doing something different every day.”
Last year, she even had the opportunity to tattoo the nurse who saved her life. “I really wanted to commemorate our happenstance meeting, and just really wanted a piece of her artwork on my body,” Amanda said. “I had her design something that I had in mind, and she did it for me. We bonded over that, too.”
Amanda is still an RN at Rapid City Hospital. “I’m still working in Labor and Delivery, and I’m just enjoying spending time with my husband and two kids — we try to enjoy as much time outside as possible in the summer.”
Katie and Amanda do their best to stay in touch — they haven’t had the opportunity to get together lately, but the two share a connection that neither takes for granted. “I think about her all the time, and I’m so grateful that she’s doing well. She is an incredibly special person, and it’s wonderful seeing what she’s capable of,” Amanda said.
“I’m still always so grateful for her,” Katie said. “I think about her all the time, how lucky I am that she was there — things could have gone very, very differently. Amanda is an amazing person, and I’m thankful that she’s part of my life.”
Katie recently had exciting news to share with Amanda — she and her boyfriend, Josh, are expecting a child.
“We are so excited! It’s one more reason I want to say thank you to Amanda. Without her, this wouldn’t have happened either,” Katie said.
For mothers with LQTS, the risk of cardiac events is reduced during pregnancy, but often increases during the first nine months following delivery. Katie and her family have planned for this and are working with specialists every step of the way to ensure she and her baby will be safe and healthy.
“There are definitely new challenges, but I think that’s true for every new mom,” Katie said. “Mine are just a little different. We’re doing everything we can to keep me and the baby safe, and we’re so excited to meet him or her.”
Written by Wade Ellett
Photos by Bob Slocum
What are your main responsibilities as a volunteer?
Right now my focus is to make blankets for patients. This is something I can do at home on my own time, which means I am still making a difference for patients while having time to care for my 92-year-old mother. When I need supplies, I come to Rapid City Hospital, pick up fleece and take it home. Then, I cut it to size, tie it into blankets and return them. Over the years I have tied hundreds of blankets. I have also returned to in-home hospice volunteering as my schedule allows and I'm so thankful the restrictions of COVID-19 have finally been lifted. Hospice volunteering is truly a rewarding experience, getting to know and visit with patients as they near the end of their lives.
What surprises you about volunteering?
Just the sheer number of opportunities available for the volunteer. Of course, it’s fun meeting and working with the other volunteers, and it also gives me a feeling of accomplishment. It’s about doing something for someone else and hopefully brightening their day during a difficult time.
What do you most look forward to on the days you volunteer?
We have a really fun group on the auxiliary board of directors, and I look forward to our meetings and conversations. It is also exciting to see just how much money the auxiliary has been able to donate to various needs within the hospital. Giving $250,000 to the Cancer Care Institute over a five-year period as well as annually donating to CMN, just to name a couple! It's possible to have such an impact because of the volunteers' support and commitment. I truly work with an amazing, selfless group of men and women who volunteer their time and energy for a much larger goal. I am proud to be listed among their ranks!
My Role
I am a Primary Care Physician Assistant at Monument Health Hill City Clinic. I provide annual wellness visits, diagnose illnesses and prescribe medications. More importantly, I act as a counselor, educator and advocate for my patients, helping them manage their health conditions, many times without the aid of specialists.
My Goal
My goal is to build trust and ensure access to quality health care for all, regardless of financial or social status. I am dedicated to improving the health and well-being of my patients in the Hill City community. Dr. Terry Graber, who is retiring this year, and I are the face of Hill City medicine, and I do not take that responsibility lightly.
My Passion
Preventive medicine, fitness, teaching and advocacy are my passions. In college as a certified personal trainer and bodybuilder, I found great satisfaction in helping individuals reach their fitness goals through proper nutrition and resistance training. As a cardiovascular and diabetes care specialist with Pfizer and Novo Nordisk, I learned from the top thought leaders in the country. This forged my strong conviction in preventing disease with a sharp focus on aggressive early disease management to improve life span, but more importantly health span. This is how I approach clinical medicine. About 15 percent of my practice is lifestyle medicine focused on prevention, weight loss and exercise. I am humbled by the constant influx of referrals from all over the Black Hills. It is gratifying to witness these huge transformations and the self-confidence that ensues knowing that they are no longer prisoners in their own bodies.
I really enjoy teaching the next generation of PAs and CNPs. I had tremendous preceptors when I went through PA school, and I try to pay that forward any chance I get. As the APP field continues with tremendous growth, we all have an obligation to be certain that quality does not suffer. Lastly, I try to be a voice for my fellow APPs. I am one of 11 members on the Monument Health APP council. I will continue to advocate for the issues that matter most to APPs at Monument Health.
My Role
I am a general medical dermatologist with Monument Health. My job is to be prepared for any skin condition that walks through the door. I take care of patients of all ages from newborn babies to adults. I also perform skin cancer surgeries and provide cosmetic services. My team and I treat a wide variety of skin concerns from common conditions such as, acne, eczema and psoriasis to more rare or complex skin diagnoses and skin cancers. Skin conditions often exist alongside other medical issues, and I work collaboratively with primary care providers and other medical professionals on a daily basis.
My Goal
When I was a medical student, I had the privilege of working under Dr. Allen Nord here in Rapid City. With every patient he would say, "What can we do to help this patient today?" I have learned to carry this question with me into each patient encounter. My goal is to use my expertise and experience to help in every way I can, every time. Each patient is unique, and I am dedicated to providing high-quality dermatologic care that is individually tailored to the needs of the person sitting across from me.
My Passion
I am passionate about my community and my patients. I always want to be the physician who patients confide in, who encourages them through difficult treatment protocols and is excited to celebrate with them once we have fully treated the skin cancer, cleared up the acne or got rid of their child's rash. Through patient education, skin cancer screenings and up-to-date medical management of skin conditions, my team and I deliver high-quality dermatologic care. Rapid City is my home, and I could not be more honored to be able to use my training, skills and knowledge to serve this wonderful community.
Dr. Hockhausen comes from a passionate medical family. She joins her father, Samuel Huot, M.D., a retired family medicine physician, and two brothers, Christopher Huot, M.D., an ophthalmologist, and Michael Huot, M.D., an anesthesiologist, in providing health care to the Black Hills region.
Monument Health offers emergency medical care at its five hospitals in western South Dakota. These hospitals treated 71,087 patients in their emergency departments in 2022. Rapid City Hospital has the busiest emergency room in the region, treating more patients each day than any other hospital in a three-state region. Stephen Dick, M.D., has spent over 30 years working in Emergency Medicine, and shared his experience answering some common questions about the emergency room.
What is emergency medicine?
Emergency medicine is the medical specialty in which physicians are equipped to handle any emergency for any patient at any time. It sounds simple, but in practice it’s immeasurably complicated. Emergency physicians are specialists who care for a wide range of injuries and illnesses, from minor to critical — and just as importantly, they have the ability to diagnose what seems minor but is actually a major problem.
When should someone seek emergency medical care?
The reality is, whenever someone is experiencing life- or limb-threatening issues or severe pain or distress, that is when you should seek emergency medical care. Typically these are new, non-chronic or sudden issues. However, in practice it’s difficult to define what is and isn’t an emergency — when patients believe they have a medical concern that needs timely attention, that’s when they should visit the nearest emergency room.
While it might be better for continuity of care if an individual saw their primary care provider for most issues, research has shown that four out of five people who called their family doctor about a sudden medical issue got the same advice, “Go to the ER.”
Stephen Dick, M.D., FACEP, has been recognized for 30 years of Emergency Medicine Board Certification by the American Board of Emergency Medicine (ABEM). He is an Emergency Medicine Physician at Monument Health Rapid City Hospital and has previously served on the Monument Health Board of Directors and as the Director of the Emergency Department.
For his initial certification, Dr. Dick completed medical school and specialized training in emergency medicine. This was followed by completion of an examination that covers the breadth of emergency medicine.
Board certification is a voluntary process and reflects a dedication to the specialty. Dr. Dick actively participates in a program of continuous learning to maintain his certification. The ABEM continuing certification process helps board- certified physicians stay up to date on current medical research and provides opportunities for practice improvement.
Are there problems that don’t warrant a visit to the ER?
Simply put, yes. However, emergency medicine is anything but simple. For many people who do not have access to primary care or preventative medicine, the emergency room is often the only place to safely receive care.
With that in mind, for patients with chronic problems who do not have acute changes and are being monitored or treated by another provider, it is usually best to communicate with the specific provider who is familiar with your case before coming to the ER. Those who are seeking specific tests, labs, CTs or MRIs, should schedule those through their provider or specialist. When a person comes to the ER, even if told to come by another provider, they will see an emergency provider who will determine what tests are necessary to complete on an emergent basis. Many tests can and should be scheduled on an outpatient basis by primary care providers.
What are some of your most rewarding memories?
There certainly have been life-saving wins and emotional “thank-yous.” I’d have to say there is a daily reward when reflecting on the fact that what we do in emergency medicine matters. The “we” is also a rewarding memory in that many of those who have chosen to be part of the ER team have been an amazing extended family as we lean on one another in trust and understanding.
Although the emergency room is always there when you need it, it’s not right for every situation. For an illness or injury that isn’t a threat to life or limb, consider a visit to urgent care.
What are some of your most surprising cases/memories?
There are too many to even consider. I have had a 30-year career in emergency medicine in which I have seen several thousand patients. Having seen so much, the one that sticks with me would not be appropriate for public comment. The worst of the worst are the cases I most remember.
It’s worth noting that for most of those presenting to the ER, they are not having a good day. For many, it’s the worst day of their lives, and I have now become a permanent memory of that day. Over the years, I have gained self-awareness of this fact and have tried to be a positive in their experience — as much as one can be in these grave situations.
What changes do you see coming to emergency departments in the future?
Over three decades I have seen huge advancement in technology, changes and challenges to operational efficiency, 180 degree changes in management standards, medication usage and many new medications and interventions to heal.
As I see it, emergency medicine’s current primary challenge is the high rate of burnout — the highest of any medical specialty. As word has gotten out of the challenges of our profession, amplified by COVID-19, there has been a significant decrease in young physicians choosing to pursue emergency medicine. Until recently, it was one of the more sought after specialties, making it very competitive.
Locally, I believe we are going to continue to see our trend of getting busier as our community grows and access to care becomes more challenging for people. It is causing us to really look at our processes and be creative with how we handle the increased volume and acuity of people needing our services.
Photos by Bob Slocum
When you walk into Monument Health Rapid City Hospital, you might find yourself receiving one of the friendliest greetings you’ve ever experienced. If that’s happened to you, then you’ve probably met Jason Plooster, better known as JP to his friends — and everyone is his friend. Because of his warmth, friendliness and positive energy, it’s no surprise that JP is a star at welcoming people. What may be surprising is that it isn't even his job. He’s an Environmental Services Technician, and while he’s great at his role, he’s also great at making people feel welcome. He loves coming to work. “I just get to high five people. It’s awesome,” he said enthusiastically.
Project SEARCH
JP, like many caregivers at Monument Health, is finding meaningful employment through a partnership with Project SEARCH. The program’s mission is to train people with developmental disabilities to have fulfilling employment through internships and through developing the skills necessary to join and thrive in the workforce.
Project SEARCH is a national organization that connects its graduates with several employers in the area. Monument Health is the largest employer of Project SEARCH graduates in western South Dakota. The program works with young people on practical job skills but also focuses on soft skills like communication, professionalism and ways to connect with people.
The program is a success. It’s great for the Project SEARCH graduates who find jobs for which they’re an excellent fit, it’s great for Monument Health because they find incredible caregivers and it’s great for patients and community members because they have the opportunity to interact with caregivers like JP.
Patients who interact with JP always walk away with a smile, but he also lends his signature sunshine to doctors, nurses and senior leadership — anyone who encounters him receives authentic, friendly encouragement. “I like working here,” JP said, directly but enthusiastically. “It’s awesome.”
Warm welcomes
JP isn’t the only Project SEARCH graduate who makes sure patients feel welcome. As a Guest Services Specialist, Berkley Kolkman makes it a priority to make patients, visitors and caregivers feel as comfortable as possible when they come to Rapid City Hospital. In many ways, Guest Services caregivers act as ambassadors to Rapid City Hospital, providing guidance, direction, information and comfort to patients and visitors alike. Berkley, a kind and gentle individual, is a perfect fit for this role and enjoys helping patients feel more at ease. “It can be hard coming to the hospital,” she said. “We give out things like neck pillows and activity books — stuff like that.” Berkley loves spending time with patients and said that she’s had the privilege of meeting some of the funniest and kindest people while on duty. She also enjoys being part of a team, and her fellow caregivers bring joy to her job as well. “I like my co-workers a lot,” she said. “All of them are really nice and supportive.”
Getting where you’re going
Moving around a hospital isn’t always easy, especially as some patients may need wheelchair assistance. Knowing where to go is only part of the challenge — when a patient needs to get from one area to another, for treatment or services, they’ll meet a Patient Transporter like Cody Brown.
Cody’s role is to ensure patients get where they need to be, when they need to be there. And it’s a duty that Cody takes seriously. “Safety is my goal,” he said matter-of-factly. He knows what is important, and he enjoys what he does, because every day brings a new experience. He can always count on two things remaining constant in his role: getting to meet kind people every day, and always hitting his step goal. “I get 15,000 steps most days,” he said with a smile spreading across his face.
The SEARCH is never over
These three caregivers are excellent representatives of Project SEARCH and show just how well the program’s graduates do as Monument Health caregivers. In fact, you’ll find graduates making a difference in Monument Health facilities across the region. And with each Project SEARCH class, new, unique and valuable skills and perspectives are sure to be rought to the Monument Health team of caregivers.
“Our Project SEARCH graduates are woven into the fabric of Monument Health. Each caregiver brings their passion, personality and whole heart to work each day,” said John Pierce, Rapid City Market President. “I truly love walking the halls of Rapid City Hospital and seeing our caregivers serving others.”
Often, you’ll see John sharing a fist bump or smile with JP.
In fact, JP has built a rapport with John. The two have nicknames for each other: JP1 and JP2.
“JP1 has an equal love and respect for all those he works with,” said John. “You’ll see him treat physicians and executives with the same friendly demeanor as anyone else. Because JP sees us as all his friends. It's something we can all take away and learn from JP.”
Written by Stephen Simpson
Photos by Bob Slocum
Custer’s Healing and Wellness Garden is an asset to caregivers, patients and community members alike. Nestled along the side of Custer Hospital, the healing garden spans 10,000 square feet and a trip around the therapy walking path reveals one surprise after another.
When Monument Health and the city of Custer opened the doors on the new $21.7 million hospital and clinic in April 2018, the vision was to make the best use of the new facility as a healing center. An outdoor space was part of that shared vision, and the healing garden began to take shape once local patron Delmer Brown was identified as the initial donor for the project. Other individuals and organizations have since made valued contributions to the project.
Joy Falkenburg, M.D., is the curator and caretaker of the healing garden. She says the space was designed to utilize sounds, sights, smells and textures to bring people into the present moment as a form of healing.
“We felt like an outdoor space was really important for the vision of Custer as a healing center,” said Dr. Falkenburg. “It’s next to the hospital so that patient rooms look out onto the garden, and patients can sit and even do rehabilitation out there.”
Dr. Falkenburg and other providers’ healing approach to medicine finds many practical uses for the garden. This includes convalescence and solitude, activity, sensory opportunities and spiritual respite.
“We have several unique plants that smell and feel different, so those can be used for stroke patients or patients with sensory abnormalities,” Dr. Falkenburg said.
On the far side of the garden, around back, a door from the hospice suite opens into a large circular area.
“It’s not uncommon that people want to die in nature and with the sunshine on their face,” Dr. Falkenburg said. The garden helps these individuals stay close to nature as they come to the end of their lives.
The first year the garden was planted, a major hailstorm wreaked havoc, but the garden has been re-planted each spring in what has become an annual event for clinic staff and community members. During this year’s planting in June, vendors, caregivers, children and community volunteers worked together to revitalize the space for another season of restorative connections with nature.
Some of the of the garden’s most special features include:
- Several seating areas, including a semi-circle pergola area.
- Two different water features.
- A children’s playhouse.
- An intention hut in which visitors can quietly reflect.
- A “wind phone” is available for people to express their grief, concern or anything else in their heart, leaving it “on the wind.”
- Five raised garden beds for growing vegetables.
- Sculptures and art throughout the garden.
- A variety of foliage from trees to shrubs and flowers meant to attract birds.
Deep roots bear rich fruits; that is nature’s way. Barb Irwin’s career with Monument Health in her hometown of Custer has developed in much the same manner. Her ties with the hospital and clinic and the community have deepened over the decades through shared experiences and dedication, reaping meaningful rewards along the way.
She has served Monument Health in various roles throughout her life, but a calling to care for the health of her neighbors drew her to nursing. More than two decades later, she is not unlike the ponderosa pines that line the C ster horizon: unwithered by the storms and better off for them.
Finding her place
Raised on a ranch near Custer, Barb was always right at home working in her local health care system. She has been with Monument Health continuously since 1997, when she started as the director of assisted living. She eventually stepped down from that role, remaining as a medication aide while she began her nursing school prerequisites.
“I went to nursing school during the day and worked nights,” she reflected. Barb became a nurse in 2005 and has been a constant presence throughout Custer Hospital and Clinic ever since. “If you want to really go back, when I graduated high school, I cooked for the hospital and collected bills at night,” she continued with a laugh.
Helping at home
Much like life on the ranch, a small town hospital is rarely boring. That’s one of Barb’s favorite aspects of the job. “What I like most about working in Custer is the variety,” she said. “If you work in a large hospital, you work in one area. Whereas in Custer you see patients in the emergency room at their worst, you see them on the inpatient side, all the way to discharge. You get to see that you have made a difference; that you have been a big part of helping them get back to their best self.”
A connection with her patients comes easy to Barb, especially since they are frequently acquainted. That’s another reward of her role.
“It’s your grandparents, your best friends’ parents, their entire family,” Barb said. “One moment you’re responding to an emergency, and the next you’re helping with end-of-life care and supporting the family.”
Barb said she is proud to work alongside the Custer physicians and caregivers to provide health care to the community.
“For a small town, we have exceptional nurses and doctors. I mean, our doctors do it all. Their specialty is anything that comes through the door. Our team of nurses and aides are a talented group of people, and they are all here because they love our community.”
Caring for caregivers
One thing about Barb that her patients may not know is that she channels her energy into caring for her team, as well. She frequently cooks a meal during her shift and serves the staff in the galley.
“I've probably done it the whole time I have worked here,” Barb said. “It depends on how busy we are — I try to cook every shift, but sometimes it’s too busy and I don’t have time.”
From freshly baked buns to soups from scratch and pot roasts of her own local Hereford beef, Barb’s culinary exploits have made her beloved by her coworkers. Recently, she was bestowed special recognition by her teammates. Debbie Risser, Manager Nurse at Custer Hospital, organized an informal gathering of staff earlier this year to show appreciation for Barb.
“You take care of us, you feed us, you just don’t quit. Your work doesn’t go unnoticed,” she told Barb.
Joy Falkenburg, M.D., stated that she believes Barb lives by a western code of devotion to her values. “I think she truly understands how health care is about the human being; taking care of the patient. Barb is a shining example of that dedication.”
During the presentation, Dr. Falkenburg recalled how when her mother-in-law was ill, Barb helped care for her. “That is the kind of person Barb is. She shows up for people, in the hospital and outside of it as well.”
No one comes and works in a ranch community without being fed and recognized — it’s part of the culture and lifestyle. The people are a part of your family because they are working beside you, so you treat them and take care of them as such, Barb explained. "I just feel like it’s part of my job every day. It’s not something I consider going above and beyond, it’s just what you do for your family.”
Western living
The culture and values of western living have informed Barb’s choices inside and outside the confines of Custer Hospital. It is still part of her life and her reprieve from what even she will admit is a difficult profession at times. As far as she’s concerned, there’s “no better way to live” than the western way near Custer, where she said the “friendly and giving” people should be prized as much as the beautiful locale.
“Ranch life is the best. It’s 24/7. Your work is your reward. If you don’t work, your animals won’t survive and you won’t have a flourishing place. There is a lot of that to take and apply to nursing,” she said.
“Everything is your job. Everything that keeps it going is everyone’s job. There’s no saying, ‘that’s not my job.’ You work as a team and the end result is a ways better than if you’re flying alone.”
Story and photos by Bob Slocum
Norma Henderson had a long, adventurous life filled with great memories.
Born in 1931 in Wessington Springs, she grew up wishing to be a pilot, and even asked her parents to allow her to take flying lessons. They said this wasn’t a proper activity for a girl, so Norma concocted other adventures. After high school, she moved to San Diego, where she worked for an advertising and public relations firm. She took solo trips to Mexico and learned to sail. Later, an old beau from high school, a young lawyer named Frank Henderson, persuaded her to return to South Dakota and be his wife.
Together they had eight children. Frank practiced law, served as a Circuit Court judge and later served on the South Dakota Supreme Court. For a number of years they ranched and operated Pine Rest Cabins near Hill City. Frank passed away in 2012, and Norma remained at the ranch, which she loved.
John Henderson, Norma and Frank’s son, moved back home to take over the ranching operations and, as her health declined, cared for Norma. He reports that one day toward the end of her driving career, she “sneaked out” to take a helicopter ride around the Hills. Her passion for flight remained strong.
A few years later, by May 2022, Norma was gravely ill, receiving home care from Monument Health Home+ Hospice. During conversations with one of her nurses, Elizabeth, she confided that one item remained on her bucket list. She wanted to fly in a hot-air balloon.
“The whole Hospice team sat down and said, ‘How can we make this happen?’ and everybody worked together,” said Michelle Sieveke, Director of Monument Health Home+ Home Health and Hospice.
Elizabeth, along with John, his sister Andrea Henderson and the Hospice staff hatched a surprise balloon flight for Norma.
On May 15, 2022, John and Andrea took Norma for an early afternoon drive in the country. They ended up at Southern Hills Golf Course in Hot Springs, where massive, colorful balloons were being readied for flight. Even then, Norma didn’t realize she would soon be boarding one of the balloons.
“When she found out she was going in the balloon, she was one happy little white-haired lady,” John said.
With help from her family and the hospice nurse, Norma scrambled into the balloon’s basket. She was joined by family friend Kristin Donnan – the only other one in the group who wasn’t afraid of heights. The afternoon was one of the Southern Hills Ballooning Association’s tethered events, so the balloon floated only several stories high during the flight. That didn’t matter to Norma – her smile grew wider with each foot the balloon ascended.
Later, Kristin compiled the photos from that day into a book, which the family signed and gave to the Hospice staff. “We just want to express our deep gratitude to the Hospice program,” John said. Norma passed away in October 2022.
Keeping the focus on living
While a balloon flight was a first for the Hospice staff, Director Michelle Sieveke said it’s not uncommon for patients to seek one last experience during care. When possible, the nurses and caregivers do everything they can to fulfill those requests. They’ve staged art shows, hosted baby showers and arranged a visit from a horse on the Hospice House patio. They even brought in an Elvis impersonator.
Other notable moments include:
- A few years ago, one hospice patient wanted to take a final motorcycle ride. With the help of Black Hills Harley-Davidson, the Hospice crew loaded her into a sidecar – they called it a bucket – and took her for a ride while blasting “Born to Be Wild" on the motorcycle’s speakers.
- Another patient, who was at the Hospice House in Rapid City, wanted to share one final anniversary with her husband. A nurse brought in her best china from home, the volunteer coordinator made them a Key lime pie, and the staff decorated the patient’s room. The couple shared a special candlelight dinner with soft music.
- One woman was completing her online doctorate program from a university, Hospice Nurse Manager Lisa Davis recalled. Hospice staff worked with the university to coordinate a ceremony, complete with cap-and-gown and an iPad video connection, so she could fulfill that dream.
“I feel like our staff really tries to capture things that are important to patients. They look at the individual and try to capture those moments,” Michelle said. “It really reflects what hospice is all about. We’re not focusing on dying; we’re trying to focus on living.”
Written by Dan Daly
Undoubtedly, you’ve heard the old saying, “You can lead a horse to water but you can’t make him drink.” Hopefully, what’s true of horses isn’t true of people as well. While a number of studies indicate that up to 75 percent of adults in the U.S. are chronically dehydrated, there’s still hope for meeting our hydration needs, and those of our loved ones. With a little more knowledge about H2O and the risks of dehydration, these hot summer months are the perfect time to improve hydration habits.
Water you doing?
Water makes up the majority of the human body — roughly 65 percent for men, and 55 percent for women. Because it’s such a significant percentage of the body, it’s crucial that people of all ages stay adequately hydrated. Every organ in the human body — and every cell, for that matter — requires water to function well. Without enough water, we can become confused, struggle to breathe, our hearts work harder, our intestines don’t function well and our kidneys become strained.
“Because water impacts every part of our bodies, dehydration can present with many symptoms,” said Sarah Fitzsimmons, PA-C at Monument Health Sturgis Clinic. “In urgent care, we frequently see dehydrated patients experiencing dizziness, headaches, fast heart rate and decreased urine output. If you are feeling dehydrated, start trying to hydrate yourself with cool liquids and get to a cool place. Seek medical care if you have concerns about dehydration or aren’t able to help yourself feel better relatively quickly.”
Dehydration doesn’t need to be extreme to have a detrimental effect. Physical and mental performance can be reduced when an individual is dehydrated by as little as 2 percent of their body weight, impairing decision making, motor function and the ability to maintain focus. Add heat into the mix, and you have a recipe for danger. “As we move into the summer months, we worry about our patients who have dehydration combined with high heat exposure. If you have been out in the heat and start feeling confused, have body aches, have a fever or start throwing up, please seek medical care right away,” Sarah said.
HYDRATION FOR ALL AGES
Although good hydration matters at every stage of life, how we stay hydrated can vary depending on age. Here are some helpful guidelines for every age.
INFANTS
The percentage of body weight made up of water is actually higher in infants — up to 78 percent, dropping to about 65 percent by the time they’re 1 year old. Even so, babies don’t need to carry around a Stanley Cup or wear a CamelBak. Unless a doctor or provider makes special recommendations, babies younger than 6 months old only need breast milk or formula. After 6 months of age, babies can begin sipping on water with meals. Keep in mind that infants can overheat easily, so try to keep them out of the hot sun and don’t dress them in more layers than you would want for yourself. Unless your health care provider has specifically recommended it, your baby does not need juice or electrolyte drinks.
KIDS
Kids should have unrestricted access to water at all times. Many families find reusable water bottles helpful for this. Remind or help your kids to fill their bottles regularly; they’ll stay more hydrated if they can drink easily. Juice and electrolyte drinks can be fun snacks but should only be an occasional treat. Most are full of sugar and artificial flavors that can contribute to obesity and dental problems. Help your kids develop a taste for plain water now, and you could help them avoid bigger problems later.
TEENS
Active teens need consistent hydration. If your teen is working outdoors or participating in warm weather sports, have a plan to keep them hydrated. If they are going to be sweating a lot, this is a situation where electrolyte replacement beverages may be helpful. Otherwise, water is best — make sure your teen is drinking enough water and discourage consumption of caffeine and energy drinks.
ADULTS
As adults, we can use indicators from our bodies to know if we are well hydrated. If you are not urinating regularly or if your urine is very dark, you need more water. Rather than getting hung up on drinking a specific amount, aim for clear to straw-colored urine when you go to the bathroom. Give yourself access to water all of the time. Any time you feel thirsty, start to get a headache, feel tired or want a snack, take a drink of water before you do anything else.
PREGNANT WOMEN
Pregnancy comes with increased water needs — moms-to-be are drinking for two, after all. Dehydration can cause significant problems in pregnancy, including early labor. Unless an OB/GYN has recommended otherwise, pregnant patients should drink lots of water, especially as the weather warms up.
THE ELDERLY
Older individuals may struggle to maintain adequate hydration. Some medical conditions require limiting daily water intake, and specific recommendations from a doctor should always be followed. Many older individuals may not realize how low their water intake is, or how much coffee they are drinking. Water bottles can be helpful to drink greater amounts of water, but if you don't like bottles, try to set out glasses at the beginning of the day to help remind yourself to drink. Aim for a full glass of water when you wake up as well as at and after each meal. You will know you are well hydrated when your urine is clear to straw-colored.
Am I dehydrated?
Two of the biggest warning signs of dehydration are thirst and urine — if you’re thirsty and your urine is a darker yellow, you’re probably dehydrated. “As a general rule, when you're well hydrated your urine will be pale and odorless. You should also be going to the bathroom regularly,” explained Sarah. “Thirst, while not always a sign of dehydration, is a good indicator for most people, and it’s a built-in reminder to take a drink of water.”
Other symptoms of dehydration include dry mouth, lips and eyes; headache; dizziness; light-headedness and tiredness or fatigue.
Flat, sparkling or fruit-infused
Flavored water is big business. A trip to most stores shows an overwhelming number of options. You don’t need to spend money on any of them to stay healthy and hydrated — tap water in a reusable bottle is your easiest, healthiest option.
However, if you truly dislike the taste of water, try gradually weaning yourself toward healthier options. Start by avoiding anything with high fructose corn syrup, which is very calorie dense and can be bad for teeth.
Carbonated or sparkling water provides another zero-calorie, zero-sweetener alternative that often comes with a light, refreshing fruit flavor. Double check the ingredients to make sure that there are no hidden sweeteners or sodium, but these can help break a soda habit and make the transition to drinking more water.
“Remember, plain old water is the best option for hydration, but if you really crave something with more flavor, your healthiest options will avoid sugar, fructose, sucralose and artificial sweeteners,” Sarah said.
1% DEHYDRATION
can lead to a 5% decrease in mental performance
2% DEHYDRATION
can lead to decreased physical performance, impairment to attention span, decision making and motor function
5% DEHYDRATION
can decrease performance by 30 percent
H2Oh yeah!
Good hydration significantly impacts the way your body works. If you don’t have good water drinking habits, now is the best time to improve. Grab your water bottle or fill a glass, and take a cool, refreshing gulp. You’re already one step c oser to being healthier and better hydrated.
WASH YOUR REUSABLE WATER BOTTLE AFTER EVERY USE.
This will help to prevent buildup of bacteria and mold. Be sure to read the manufacturer’s instructions to determine if the water bottle can be cleaned in a dishwasher or if it needs to be washed by hand. Avoid filling it with sugary drinks — sugar can provide a food source for bacteria and mold, something nobody wants a swig of! If you do put milk or juice in your water bottle, rinse it out thoroughly after each use. Likewise, if you share your water bottle with others, be sure to wash it after each use.
Written by Stephany Chalberg
Wade and Ruth Strong were visiting the Black Hills with the hope of fulfilling a bucket list dream — visiting Mount Rushmore. For those that live near the National Memorial, this may not seem like a challenge, but it was far from easy for the Strongs.
“My wife and I are in our late 80s, and we were on a bus trip from Pennsylvania,” said Wade. “We’d been having some issues and visited a few emergency rooms along the way.”
One of those visits was at Monument Health Lead-Deadwood Hospital under the care of Nurse Practitioner, Christine Duerksen.
“After his initial assessment I told him that I would do my best to get him feeling better so he could be on his way,” Christine said. “He looked at me and tears welled up in his eyes, he said, ‘I came here to see Mount Rushmore. It’s on my bucket list. I’m not sure I’ll ever get to see it now.’”
Christine wasn’t willing to let Wade miss out on his dream. Instead, she told him that she would do everything she could to help turn this dream into a reality. And that’s exactly what she and her team did.
“Everyone I work with here, we’re like one. big family,” Christine said. “I come from a small town so when someone needs something, you just do what you can to help. I’m glad we could help.”
Christine and her team called every taxi and tour company they could think of, but kept striking out. That is, until Lead-Deadwood Paramedic, Julie Martin, had the idea to call someone that she knew could help — her son.
“My mom called and she was like ‘do you want to do something?’” Dyllen Martin said. “I told her, ‘well, yeah, but you have to explain it first.’”
Dyllen, a 19-year-old college student, was home for the summer, but hadn’t yet started his summer job with Sturgis Fire and EMS. He listened as his mom explained how an entire team of caregivers was trying to help the Strongs get to Mount Rushmore. Julie asked if he would be willing to act as a tour guide for the day.
“When I first met them they were kind of in shock I guess. They were happy that I was there and they could see Mount Rushmore,” Dyllen said. “He just made our day,” Wade said. “Dyllen took us out for maybe five or six hours.”
Mount Rushmore
“Mount Rushmore met all of my expectations — my bucket list was fulfilled,” said Wade. “When we got there, our bus tour was leaving. I was in a wheelchair and he pushed me up there. I would have never made it without him.”
Dyllen helped the Strongs tour through the memorial, pushing Wade’s wheelchair and helped the couple to the amphitheater to watch an educational video. After that, the adventure and Black Hills tour continued.
“I gave them a couple options after Mount Rushmore,” Dyllen said. “We took the Needles Highway drive through Custer, made a few stops so they could take more pictures and see the wildlife.” It was the trip of a lifetime and now, they have memories to share.
“They had an older phone that didn’t really take pictures, so I took a few and sent them to their grandson,” Dyllen said. “I did print out a few and mailed them as well.”
Thinking back on the eventful day, Wade said, “It was the most wonderful day I ever had.”
Written by Stephany Chalberg
Photo by Dyllen Martin
At almost 22,000 feet of elevation, climbers on Mount Everest ascend Lhotse Face toward Camp III. What starts as a flat walk leads to an icy incline, where climbers will clip into fixed lines — ropes that are permanently in place to facilitate climbing — in order to ascend what is essentially a 4,000 foot icy slide. Ice and rock, dislodged by climbers moving above, careen downward.
As Trauma Surgeon Jacob Weasel, M.D., approached the Lhotse Face, one of those rocks, roughly the size of a billiard ball, hit him on the left side of the chest. His experience and medical knowledge told him that while the impact hadn’t broken any ribs, it had caused severe bruising. But there’s only one thing to do on Mount Everest — just keep going.
“In the aftermath, after I’ve come back down from the mountain, I know how crazy that is,” said Dr. Weasel. “A foot higher and four inches to the right, it impacts my heart and I’m dead. If it had hit me in the throat or face, I wouldn’t have come off the mountain alive. Instead, I just continued on to Camp III.”
It’s a long way to the top
Everyone knows that it’s a challenge to climb Mount Everest, but they may not grasp just how complicated it can be. It’s a multistage process that can take up to two months. The first step is getting to Everest Basecamp — a one- to two-week journey in and of itself. From there, it takes an average of 40 days to reach the summit of the tallest mountain in the world.
The route up Mount Everest, for those braving the climb, is broken up into four camps, not counting Basecamp. A process of ascending, acclimatizing to the thinner air, descending and then climbing again is the only way to prepare for the final push to the summit from Camp IV. Finally, if weather and timing cooperate, climbers can make a bid for the summit, which can take anywhere from eight to 16 hours.
Dr. Weasel departed Rapid City on April 10, and summited Everest on May 17, 2023 — close to the average time to complete the feat.
You may have seen photos of lines of people leading up Everest. These may make it look like immeasurable amounts of people have reached the summit, but if you were to amass a group of everyone who had been to the top of Mount Everest, you’d have a relatively small club. By the end of the 2023 climbing season, the total number of climbers who have summited since Edmund Hilary and Tenzing Norgay became the first confirmed summiters in 1953, sits at around 7,000. To put that in perspective, that is less than one tenth of one percent of the current world population.
“This is an opportunity that few people get,” said Dr. Weasel. “I’m grateful for it.”
Dr. Weasel has developed a solid resume of mountain climbing before summiting Mount Everest (29,032 ft). His first experience mountaineering was climbing Mount Rainier (14,411 ft) when he finished his undergraduate degree. Since then he has tackled 14ers — mountains reaching 14,000 feet above sea level — in Colorado, as well as Cloud Peak (13,171 ft) and Grand Teton (13,775 ft) in Wyoming. He traveled to Ecuador to climb Cotopaxi (19,347 ft) and Chimborazo (20,549 ft) and to Tanzania to summit Kilimanjaro (19,341 ft).
Why Mount Everest
There are a lot of reasons why people climb Mount Everest. Some need the biggest challenge they can find, others are seeking thrills. For some, the mountain is laden with meaning and significance. Dr. Weasel loves climbing mountains, but Mount Everest was never on his metaphorical horizon. That is, until he realized how he could use the mountain to do good.
“It’s important to me to give back. That’s why I took a position serving as an Assistant Dean for Diversity and Inclusion at the University of South Dakota Sanford School of Medicine,” Dr. Weasel explained. “One of my goals is to try and recruit and encourage native kids to pursue careers in health care and related fields.”
The Everest trek provided the physician with additional avenues for helping others. He hoped he could set an example for native youth, to show them that they are equally as capable as anyone. “Whether we’re talking academics, the professional world or yes, climbing Mount Everest, I want all native people to know that they’re capable of accomplishing anything.”
Leading up to his departure for Nepal, Dr. Weasel created a nonprofit called the Wopila Project. Wopila is a Lakota expression of gratitude for everything that life offers, for existence and for the blessings in every moment. “The goal is to cultivate gratitude, to inspire hope and to work together to create a tangible impact in people’s lives,” he said. “My hope was that I could use my Everest climb to raise awareness of our current projects and get people involved. I’m happy to say that there has been positive feedback, and I’m excited to keep the momentum going.”
Dr. Weasel’s nonprofit, the Wopila Project, is currently raising funds to build a playground at Lakota Homes, a housing community in Rapid City that serves the local Native American population. The plan includes surrounding the playground with informational displays of each of the seven traditional Lakota values; Prayer, Respect, Wisdom, Compassion, Honesty, Generosity and Humility. Once completed, the next goal is to construct sustainable women’s health clinics in Nepal in order to provide obstetric and gynecological care to help the disparity related to women’s health in the rural areas of the country. To learn more about the Wopila Project, visit www.wopilaproject.com.
A view from the heavens
After arriving at Camp IV, Dr. Weasel and his Sherpa, Lhakpa, took a rest day. They ate and hydrated, and tried to rest and sleep as best they could. They stepped out of their tent at 10 p.m. the next night, to perfect conditions — clear skies with no wind.
Despite the evening start, there was already a line of people, but Dr. Weasel and Lhakpa passed climbers and pressed onward. “The mountain just keeps going. It goes on and on and on. It never seems to end and you just keep climbing,” said Dr. Weasel. “And I kept occasionally looking at my watch, asking myself, ‘when is the sun going to rise?’ Because I was freezing cold, and wanted nothing more than to see the sun rise.”
In May, the average temperature at that elevation is -13 Fahrenheit. It can get much colder, and wind chill can lower that temperature significantly. Luckily the air was pretty still for Dr. Weasel. While the rising sun wouldn’t raise the temperature significantly, every degree counts on Mount Everest, and the psychological benefit of sunrise would have a dramatic effect.
Dr. Weasel explained, “You just keep. climbing and then you get to the point where the sun finally starts to peek out. And it is breathtaking. That was probably the most beautiful thing I've ever seen in my life. It is amazing watching the sun rise over one part of the valley and then look to the other side and seeing the perfect pyramid of Everest’s shadow being thrown onto the valley. And you cry because it is that beautiful. Then your tears freeze to your face, but it is literally amazing.”
You might expect a similar sense of awe at the summit, but for Dr. Weasel, the experience was somewhat muted. He said that the view was incredible — from the top you can see 200 miles of the world spreading out beneath you. Across the valley to the northwest is Cho Oyu, which is the eighth-tallest mountain in the world. Looking Southeast you’ll see Makalu, the fifth-highest, and closer still is Lhotse, the fourth-tallest.
That last view, of Lhotse, is partially responsible for Dr. Weasel’s more muted response to the summit of Everest.
“The summit was good, but I was there to climb two mountains,” Dr. Weasel said, explaining his plans to climb Lhotse following his completion of Everest. “When I stood on the summit of Everest, I didn't fully appreciate it because I was so disciplined at that point that in my mind, I was only 25 percent done.” Mentally, he was already working on the descent back to Camp IV, from which — if things went according to plan — he and Lhakpa would then summit Lhotse the next day before beginning the trek back to basecamp.
Unfortunately, a number of considerations conspired against the two men, and in the end the second climb didn’t happen. One of the reasons likely being the amount of time Dr. Weasel had spent in what is known as the Death Zone.
The Death Zone
As a general rule, human bodies work most efficiently and effectively at sea level. At high altitudes, bodies become less and less efficient. For those that want to summit Mount Everest, they have to enter — and stay in — what is known as the “Death Zone.” At this elevation, above 8,000 meters or 26,247 feet, the air has so little oxygen that the human body will begin slowly dying, one cell at a time, even when using supplemental oxygen.
“Making it to the top is everyone’s goal, but once you do you’re not done. You still have to descend safely,” said Dr. Weasel. And while it may seem like it should be easier to come down from the world’s highest peak than it was to go up, more accidents occur during the descent. A combination of exhaustion, hypoxia, a caloric deficit and hypothermia — combined with the inherent risks of avalanches, falls and other injuries — make coming down a challenge unto itself.
As climbers’ brains starve for oxygen, their judgment and decision-making skills get progressively worse. As the lungs struggle with oxygen deprivation, the risk of heart attack and stroke increase, as does the likelihood of a high altitude pulmonary edema. This happens as the body produces additional hemoglobin in an attempt to compensate for the lack of oxygen. As it thickens the blood, it can also cause an accumulation of fluid in the lungs that comes with shortness of breath, a sense of impending suffocation and persistent coughing.
Likewise, if the brain doesn’t get enough oxygen, it can cause swelling which leads to high altitude cerebral edema. Symptoms include nausea, vomiting, impaired judgment and difficulty thinking. At worst, it can lead to delirium in which climbers may not remember where they are, begin destroying clothing and gear or speaking to people who aren’t there.
Most climbers are advised to not remain in the Death Zone longer than 24-48 hours. Dr. Weasel estimates that he spent about 63 hours, between his arrival at Camp IV, summit and descent.
“I recognize that with that much time in the Death Zone, at any point my body could have just said, ‘no,’ and given up,” he said. “I could have just collapsed and died.”
Although he returned safely, that doesn’t mean that the Death Zone didn’t take a toll on the physician. “I definitely hallucinated on the way up and on the way down. I heard voices of my team members on the way up,” he said. “On the way up, and even more pronounced on the way down, I saw the faces of my children, when they were younger, and the face of my wife coming out of the rock.”
Hallucination is a common, and temporary, symptom of hypoxia. It’s something that most climbers will have to endure on Everest, and after descending into a more oxygen-rich altitude, the symptom goes away.
“I didn't consider the actual physiological effects of what was happening. I knew I was hallucinating, and just thought, ‘Hmm, that's interesting.’ And I just keep working my way down the mountain.”
“I have always found there to be a lot of similarities between surgery and mountaineering. In both cases you have a plan, but your plan never goes exactly as you anticipate, so you have to be agile and flexible enough to recognize and adapt to the situation as it's presented to you. There’s always a balance of risk and reward —you're trying to minimize the amount of risk and to provide the best possible outcome. Sometimes when you're on the mountain you’re dealing with life or death decisions. Those are high stakes, and they are similarly high during a surgery.”
The man on the mountain
It may seem odd that someone who had just summited the tallest mountain in the world would feel disappointed, even angry, that he was turned back from the fourth-tallest. Especially after experiencing hallucinations in something called the Death Zone. But Dr. Weasel has a self-described stubborn streak. While that streak leads to disappointment when he’s turned back from a goal, it’s the same quality that empowers him to climb mountains — and to reach where he is in life now.
Dr. Weasel, an enrolled member of the Cheyenne River Sioux Tribe, knew from a young age that he wanted to become a surgeon. “When I told people that I planned to become a surgeon some people told me that there’s no way that that’s ever going to happen, that it’s not even possible,” he shared. “But the more that people would tell me that something wasn’t possible, the more that it spurred me towards accomplishing a certain thing.”
That stubborn streak would propel him up mountains like Cotopaxi and Chimborazo, where he experienced conditions he described as horrendous, including white out visibility and 50 mile-per-hour winds that pelted his face with ice which he likened to being in a sandblaster. Even before that, it spurred him on through his undergraduate education, medical school and surgical residency, an experience he likened to training for mountains.
“Surgical residency was super helpful for mountaineering. It was probably the best training that I could have had, learning how to operate with little sleep, learning how to operate mentally and physically on very little food and just taking a beating and having to come back and keep going,” he explained. “When you’re working 80 hours a week in residency and you still have a family, and you still have to read and prepare and do all those things — having experienced that kind of mental exhaustion on a long-term basis is super helpful when you’re on a mountain.”
There’s always another mountain
After climbing the tallest mountain on earth, you might think Dr. Weasel would hang up the mountaineering goggles and retire his crampons, but that isn’t the case. He said, “I love mountains, and so climbing them will be a part of my life for as long as I’m able.” He’s already working on his next great challenge — becoming the first enrolled member of a Native American tribe to reach the top of the Seven Summits. This entails climbing the highest mountains on each of the seven continents: Mount Everest, Aconcagua, Denali, Kilimanjaro, Elbrus, Mount Vinson and Puncak Jaya.
He’s already checked Mount Everest and Kilimanjaro off the list, and is looking forward to returning to Mount Denali in Alaska, the highest peak in North America, with a summit elevation of 20,310 feet above sea level — he almost summited in 2022 before his guide turned him around due to dangerous weather.
“I might as well save Mount Vinson in Antarctica for last, and then ski to the South Pole,” he said with a smile. “Because then, if I do that, I’d have to do the North Pole, making it an Explorer’s Grand Slam.”
Less than 100 people have completed this assemblage of summits and treks, and it’s easy to think of the challenges and adversity and ask, “Why?”
Maybe, as George Mallory said of climbing Mount Everest, “Because it’s there.”
Or perhaps, as Dr. Weasel said, “There’s an opportunity to inspire and help others while doing something that I love. That’s gratitude coming full circle.”
Written by Wade Ellett
From bad to worse
When long-haul trucker Don Wood got sick while on the road to Colorado in December 2021, he couldn’t anticipate the hardships and challenges that were ahead of him. When he left his home in Spearfish, he was perfectly healthy. By the time he returned, however, he was sick, and it was quickly getting serious.
“I left on Monday to make my deliveries to lumber yards in Colorado and Wyoming, and by the time I got back that Saturday, I wasn’t feeling well at all,” he said. As soon as he got home that day his wife, Patty Wood, helped get him to the hospital to be tested for COVID-19. “I got tested and sure enough it was COVID-19,” Don said, “When that came back, they hospitalized me right away.”
From there, things went from bad to worse for Don, as he developed some of the most severe complications from COVID-19. Just four days after Christmas, he went into cardiac arrest. “He was in Spearfish hospital for the first couple weeks, then he coded, so they sent him to Rapid City,” said Patty. At Rapid City Hospital, he was taken to the ICU and placed on a ventilator. He was there for five-and-a-half weeks.
During the height of the pandemic, the mortality rate for COVID-19 patients on ventilators was between 50 and 97 percent. Don was fighting for his life, and the odds were against him. Even if he did survive, his doctors were concerned about potential long term brain damage.
“His neurologist ordered an EEG. There was very little brain activity, but I saw some. It wasn’t nothing,” Patty said. “So, after talking with the doctor, she recommended we wait a few more days and do another EEG. We just weren’t ready to give up on him.” That time was enough for Don to wake up. “I know a lot of people don’t believe in miracles, but we do. We got seven miracles, and Don waking up was the first.”
Difficult decisions
Don moved between nine hospitals and clinics in nearly as many months. Either to receive more specialized care or because there weren’t enough beds due to the pandemic.
He was airlifted to Scottsbluff, Neb., where his health began to turn around, even though things looked grim when he arrived. The receiving physician had to perform a bronchoscopy. His lungs were so full of fluid that doctors didn’t have high hopes of recovery. “The person who does the life flights came to visit me. He didn’t think I was going to make it when I came in, and he ended up giving me his cap. He said he was rooting for me.” Don pointed to the red baseball cap he was wearing and continued, “I call it my $51,000 cap!”

Don pointed to the red baseball cap he was wearing and continued, “I call it my $51,000 cap!”
It was in Scottsbluff where they were finally able to get Don back on solid food. “When I went into the hospital, I weighed 230 pounds. When I finally woke up and they took me off the ventilators, I had lost 100 pounds,” he said.
After he stabilized and was able to eat again, the hospital was ready to discharge him. “I was in a wheelchair. I was so weak, and I couldn’t walk. They said there wasn’t anything more they could do for me, and they were discharging me.”
It was recommended that Don be placed in an assisted living facility. For the Woods, that was completely out of the question. "We said no,” Patty said. “He didn't want to be in a nursing home, and I didn’t want him there either. He wouldn't have been happy that way.” They decided to try physical therapy. This eventually brought Don back home to Spearfish, where he started physical therapy at Monument Health. “That was when we really started to notice a difference,” Patty said, “We came here, and Don was in a wheelchair, and 14 months later he was walking.”

Starting recovery
Matt Weigel, Physical Therapist, and Meagan Stephens, Occupational Therapist, at Monument Health Rehabilitation in Spearfish were part of Don’s recovery team. Matt said when Don came in he wasn’t sure what to expect. “COVID-19 was a new thing and people in Don’s position often wouldn’t survive to start physical therapy. We didn’t have a ton of data.”
Matt started with small, attainable goals. Don was on six liters of oxygen a day, and Matt didn’t want to push him too far, too fast. “We would just do exercises lying down, then a couple standing exercises,” Matt said. “Eventually, we were able to use some of the leg machines. After that, we started to see Don walking a little bit, but not a ton.”
Don’s lungs were particularly concerning. COVID-19 had done a lot of damage, and there was a lot of scarring. Matt said, “He was on quite a lot of oxygen when he came in. His lungs aren’t ever going to be how they were before he got sick, but I didn’t expect to see anywhere near as much recovery as we did.”
After Don’s physical therapy, Meagan would take over for his occupational therapy. Like physical therapy, occupational therapy went slowly. “We were on a separate schedule because he could not tolerate two therapies in a row, so PT and OT were always on separate days,” she said. “If we were back-to-back, therapy wouldn’t have been as effective.”
While Matt focused on Don’s strength, mobility and endurance, Meagan helped Don learn how to do everyday tasks to help make him more independent. “Patty was helping Don with 90 percent of his active daily living tasks. Things like helping him get dressed, getting in and out of the bathroom, showering — all the small things we take for granted,” said Meagan. “We wondered if we would ever get him back to that full independence. Could we get him to the point where he was able to tie his shoes without getting exhausted? By October we had him doing all those things for himself.”

From small successes to big wins Don was hitting his goals, and the focus shifted from seeing the most he could hope to do, to seeing how far he could go. “We started with these very basic goals, like standing up from furniture, or having him walk across a room on his own,” Matt remembered. “And Don was putting in the work and hitting all of these goals. These were just basic things a person needs to do every day, but they seemed lofty at first.”
As Don started to achieve these goals Matt said more things suddenly seemed possible. “I started to ask questions like, ‘Can you make yourself lunch or walk to the mailbox?’ ‘Can we actually get outside with oxygen?’ ‘Can you get down the stairs?’ It opened up my eyes. We’d talk about what he wanted to accomplish, and we kept going and broke past what we thought was the top limit.”
Don remembered a very special milestone he was able to reach. “I had whiskey and my coffee that I wanted to be able to reach. It was really high up, and I just wanted to be able to stand tall and balance on my own to get it. I was able to finally reach up there and get my whiskey, my coffee and my filters on my own.”
Meagan remembered setting that goal. “We were going to get the whiskey behind the coffee. It’s funny but that's a lot of what occupational therapy looks like, getting back those little things we do every day.” She and Matt worked as a team to reach their goals, often checking in with each other to see what milestones Don was able to achieve. Another major achievement sticks out in Meagan’s mind. “I'll never forget the day when I saw their car pull up and Don stepped out of the driver's seat and grabbed his oxygen. I ran to Matt, and said, ‘Don just drove here!’ He walked in so proud.”
Patty looks back at that time now and remembers the support she had from her family, the work Matt and Meagan put into bringing some normalcy back into their lives and her husband’s strength. “You know, it's funny, he had the right attitude, and he worked so hard at it. He really wanted to get better, and he was used to being a normal person. It was hard for him to lose that, so he worked hard to get it back.”
Meagan agreed and said that it can be a hard battle. “When that independence is taken away from you, it can be frustrating and tiresome. To be able to retrain your body, to regain that strength is a huge victory.”
Taking a trip, whether a weeklong vacation or just a weekend getaway, is a great way to decompress, refresh and celebrate. But anyone who has had a trip go awry because of health issues can tell you that a dream vacation can become a nightmare when you don’t feel well. Whether it’s food poisoning, allergies or misplaced medication, health issues can derail any trip. Luckily, there are ways to make sure that your travels are smooth sailing.
Eating can be a big part of travel. Whether you enjoy fine dining or food trucks, it’s important to enjoy what you eat while on vacation. “I often advise my patients not to worry about losing weight while on vacation,” said Rachel Van Den Top, Clinical Dietitian. “I think your mind should be focused on the exciting things you’ll be doing, new places you’ll see and the yummy foods to try rather than the number on the scale during vacation.”
Rachel also warns travelers to be on the lookout for what she calls, “travel tummy.” That can be anything from inconvenient abdominal discomfort or more serious travelers’ diarrhea. “This can be a result of a difference in climate, different sanitary practices or simply the stress from travel. If you know you’re going to an area where the tap water is contaminated, it is especially important to plan ahead and have bottled water available. You also will want to avoid drinks with ice in them, as the ice may be made from the contaminated water,” Rachel explained. Researching beforehand can help you learn if an area has water that you should avoid or if you need to be vigilant about unsanitary food practices. This will help you avoid travel tummy as well as more serious conditions such as hepatitis A or typhoid, or illnesses caused by bacteria,parasites and viruses.
Travelers should also be on guard against dehydration, which can pose serious risks. Even in areas where water may be contaminated, it’s important to stay well-hydrated, especially in warm climates. “Do your best to have a water bottle on you at all times or bottled water nearby. You can set a timer on your phone to remind you at a certain time of the day to catch up on water intake,” suggested Rachel. “Since you will be eating different food than you are used to, and in a different routine, it is important to drink adequate water to keep your bowel movements regular.” In areas where water may be contaminated, you will want to drink bottled water or use a water purification method.
Always keep your medications with you when traveling.
Although airlines strive to make sure everyone’s checked baggage arrives where it should be on time, everyone knows someone who has lost luggage — keep your medications in your personal item or in your carry-on luggage to prevent any issue with lost baggage. Medications should be kept in their original, labeled containers from the pharmacy. Remember to pack a cooler for medications that have to be kept cold, like insulin.
If you forget to get your medications filled prior to departure, or your medicine is lost or damaged, contact a pharmacy in your travel area. “Typically, when traveling within the United States, most prescription medications can be transferred over the phone to a pharmacy of your choosing. Special rules and restrictions do apply, especially for controlled or DEA scheduled medications, that may make this process more complicated. Be mindful, higher copayments may also occur when filling at an out-of-network pharmacy,” said Stephanie.
These suggestions can help you avoid getting ill on your trip, but what if you have medication that you need to continue taking during your travels? Pharmacist Stephanie Magbuhat, PharmD, suggested having all prescription medications ready well before your departure date. “The most important piece of advice I can offer is to plan ahead,” said Stephanie. “Long before your travel date approaches, call your preferred pharmacy and make sure you have refills on all your medications, and confirm you will have enough to get you through the entirety of your trip, as well as a little extra to account for any flight or weather delays.” Most insurance companies will allow at least one vacation override per medication per calendar year if the refill dates don’t quite line up. “Just call your pharmacy with your specific travel dates, and they will happily call your insurance company if needed,” added Stephanie.
It’s not uncommon to throw routine out the window when traveling, but remember that medications must be taken as prescribed. “Remember which medications need to be taken with food and which need to be taken on an empty stomach. Be mindful that some medications shouldn't be mixed with alcohol,” said Stephanie. “If you are traveling across multiple time zones, or fear you can't replicate your normal routine, feel free to call your pharmacist for specific recommendations.”
If traveling internationally, you will need to take additional steps to prepare. Some foreign countries may have additional travel requirements, such as required or recommended vaccines or medications for protection against common pathogens. Some prescription medications may not be available, or may even be illegal, in some countries. “To be sure the medications you are traveling with are permitted, and you have all the correct documentation, you should always check with the embassy or consulate in that county prior to departure, especially if traveling abroad with DEA scheduled medications,” advised Stephanie. For specific guidelines, the CDC’s website is a reliable source of information, or ask your primary care provider for guidance.
Depending on your destination, you may not have access to the same over-the-counter medications that you do at home. It may be worthwhile to pack your own, especially if you have seasonal allergies, a sensitive stomach or are prone to headaches. Stephanie suggested, “In addition to basic first aid supplies, your travel kit should also include medications for the following ailments: diarrhea, heartburn, allergies, motion sickness, pain and fever relief, constipation and insect bites. If you are interested in specific recommendations, contact your pharmacist for a personalized list geared toward your destination and in accordance with your prescription medications to assure there are no conflicting drug interactions.”
If you’re flying into a different time zone, you may also experience jet lag, which is a temporary sleep problem caused by your body’s circadian rhythms — or internal clock — not adjusting to your new destination as quickly as you travel. Symptoms include daytime fatigue, upset stomach, difficulty staying alert and a general unwell feeling. The farther your trip takes you, the more severe your symptoms may be. While there is no single, surefire way to prevent jet lag, there are steps you can take to reduce the likelihood of experiencing it or reduce your symptoms. You can start by getting plenty of rest before your trip, since starting your trip already sleep deprived will make symptoms worse. Try to sleep on the plane if it is night where you’re going but try to stay awake if it’s daytime at your destination. You can also try to gradually adjust your schedule before you leave — if your trip will take you east, go to bed an hour earlier each night a few days before you depart. If flying west, reverse it and go to bed one hour later. Once you reach your destination, keep your routine with the local time, including when you go to bed and get up, as well as when you eat your meals. Staying hydrated can also help counter the symptoms of jet lag.
Whether you’re traveling around the globe, across the country or just down the road, your getaway should make you feel awesome, not awful. Taking these steps can help you ensure that you don’t get a case of travel tummy, suffer from too much jet lag or just wish you were back home.
On Aug. 23, 1988, Melody Rindahl was murdered by her husband, Randy. She was a victim of domestic abuse, but to those that knew and loved her, she was so much more. She was a beloved sister, a singer with a beautiful voice and a devoted friend. She was also a mother, despite the fact that her son had not yet been born.
When paramedics arrived on the scene, they found seven-and-a-half months pregnant Melody, not breathing and without a pulse. They knew in that instant she wouldn’t survive. And while this might sound like the end of a story, it’s actually the beginning. Because though Melody’s life was ending, the most important thing in her world would live on — her son.
His journey certainly didn’t start in a positive way. His biological mother was kept alive by CPR until the paramedics could get her to the hospital. There, she was sustained by a life-support system until he could be delivered by emergency cesarean section. Despite the quick action of the paramedics on the scene, he had suffered oxygen deprivation and there were concerns about his health.
Because he was premature and due to the traumatic nature of his birth, he had to stay in an incubator, and twice required CPR. The outlook wasn’t great — there was a very real chance that he would never be able to walk or talk.
Melody’s experience is not a new one, and sadly, it isn’t the last of its kind. Her story, voice and memory are remembered and honored in a short film by Emmynominated Director, Jason Clemons. To watch Melody’s Story click here.
Loni Bedard, CNP, cared for Ben while he was in the NICU. Despite 39 years at Rapid City Hospital, she’s never seen another case like this. “I can still remember seeing him lying on the radiant warmer,” she recalled. “Just a fragile, preterm baby who needed so much support in the NICU to survive. He was a miracle baby.”
“At first, we didn’t know if he was going to survive,” said Patsy Ericks, Melody’s oldest sister. “But he did much better than they expected and he came home with us in 23 days.” The baby boy was named Benjamin Lee; the name Melody had picked out if her baby was a boy.
Patsy credits the physicians, nurses and other caregivers for Ben’s quick recovery. “Dr. Thiessen delivered Ben, and Dr. Kovarik was the neonatologist that took care of him after birth,” she said. “And of course, the NICU nurses that looked after Ben were amazing too.”
This was long before the hospital would become part of the Monument Health system; at the time, it was Rapid City Regional Hospital. Obstetrician Hubert H. Theissen, M.D., and Neonatologist Stephen Kovarik, M.D., have both since retired. Many of the nurses who treated Melody and Ben have also retired.
Loni Bedard continues seeing patients as a certified nurse practitioner, and despite her tenure at Rapid City Hospital, she’s yet to have another case that has stuck with her like Ben’s. “I knew Patsy, Curt and their kids. We went to church together. Between the trauma, the severity of the situation and knowing the family, I had a lot of emotions. It’s not something I could ever forget.”
Despite the tumultuous beginning, Ben grew up a happy, healthy boy. He started his life as a ward of the state, but Patsy and her husband Curt were quickly granted an interim guardianship over Ben, who they took home and raised as their own. Soon after, their guardianship was made more permanent, and one and a half years later they officially adopted him. “That was just a formality though. Ben was already part of our family,” said Patsy, who became Ben’s adoptive mother. Ben’s arrival in the Ericks family was unexpected, but he fit perfectly. The infant found himself in a home with three older sisters, Clarissa, Charity and Cameo. “I was four months old when Ben came to live with us, so I’ve never known anything different,” said Cameo Haugen. “There were a lot of times growing up that people assumed we were twins.”
Good families tend to find their own balance, their own equilibrium. It was no different for the Ericks family. Clarissa was 11 years old, and Charity was 6 when Ben joined the family. With 4-month-old Cameo a recent addition as well, the balance of the family shifted. “Us older girls — without ever really thinking about it — took on one of the babies,” said Charity Hathaway. “Ben was my baby. Whenever he needed something, it was me who got it for him. Looking back at the family pictures, I always had Ben in my lap or we were sitting next to each other, arms around one another. From day one, we had a very, very close connection and bond with each other. We still do.”
That closeness didn’t just affect their family life, it also had a profound effect on Charity’s career path. She knew at a young age that she wanted to work in health care so that she could help others in need. “I vividly remember the night that Ben’s mom was shot. I remember the policeman coming to our door. I remember our grandma coming over to stay with us,” she said. “It truly impacted the future of my life. I remember visiting Ben in the NICU and telling my mom, ‘I’m going to be a nurse someday because I want to take care of people that need me.’” Charity did just that, becoming a Registered Nurse and earning her BSN. Though she no longer lives in Rapid City, she worked at Monument Health for 17 years, with the majority of her career in Labor and Delivery.
Despite worries that lack of oxygen and blood flow perfusion could have lifelong debilitating effects, Ben was not only a healthy child, but he grew into an athlete who played high school football and was even signed to play at the collegiate level. Instead he chose to serve his country, enlisting in the South Dakota National Guard, deploying to Afghanistan in 2013 for Operation Enduring Freedom, and to Cuba in 2022. “There was a lot of worry when I was a baby, but the only problem I’ve really had was a little asthma,” Ben said with a chuckle. “And what kid these days doesn’t have a little asthma growing up.”
Having never truly met his biological mother, Ben only knows Melody through the stories his mom, grandmother and sisters have shared with him. “I’ve lived a good life with a great family, and there is always — in the back of my mind — a question of what if that never happened? What would my life have been like if I had grown up in the shadow of that abusive relationship? I would have had a very different upbringing,” Ben explained, thoughtfully. “So I know my biological mom through their memories, and I know she loved me, but I’m grateful for my family that raised me.”
When talking about family, it’s clear how important the people in his life are to him. “He’s probably the best husband and father anybody could ask for. He’s the complete opposite of his biological father,” said Cameo. “He’s loving and caring, and dotes on his wife and his children. He’s amazing.”
To Ben, Curt Ericks is his dad — his biological father simply provided genetics. He said, “I had a great role model growing up with my dad, and I think I strive to be like him, not the other guy. I think being a role model is very important, and I had the best. I just focus on being a good husband and role model to my boys.”
“I want them to see what a healthy marriage is and what it should be. I know I had that growing up with my family,” he added.
You can’t untangle the life of Ben Ericks from the murder of his biological mother. Patsy said, “This story became a huge part of our entire family. When something like that happens, everybody responds differently, and you never forget.” And while that’s true, Ben’s story isn’t a tragic one, even if that’s how it started. Instead, it’s the story of a kid who grew up in a good family — his family. He was a great brother, and grew into the kind of man any parent would be proud of; a good husband, a good father and a man who cares about the people around him.
“I think the story of my life can give a different perspective on what family is and how important it is,” Ben said. “Family isn’t just who your biological parents or siblings are. It’s the people that are there for you. The ones who love you.”
Written by Wade Ellett
Photos by Bob Slocum
My Role
I work with a team of skilled professionals at the Monument Health Orthopedic & Specialty Hospital. We provide a variety of musculoskeletal care for our community. This involves evaluating patients with acute and chronic orthopedic concerns in our clinic, as well as assisting the surgeon in the operating room.
My Goal
My goal, and that of orthopedics, is to help patients improve or restore function so that they can get back to their normal routine. I try to understand patient expectations and use the tools of orthopedic medicine to help meet their needs as a provider. My goal for the next year is to continue to mentor new APPs in orthopedics to become better providers, which ultimately helps deliver high-quality care for our community.
My Passion
I have been involved with health care in a variety of capacities over the last 25 years, and orthopedic care has always given me joy. This is a field of medicine where I get to see patients typically improve the quality of their life. To be able to see a patient come back to the clinic after surgery and show me they can walk better or even lift their arm over their head when they couldn’t before makes me happy. Knowing that, as a physician assistant, I was able to help get the patient to that point of life satisfaction is my passion.
Advanced Practice Provider (APP) refers to physician assistants (PA-C), certified nurse practitioners (CNP) and certified registered nurse anesthetists (CRNA). Because of their advanced training, APPs can do many of the same things a physician does. Patients benefit from having both their physician and their APP working together on their care.
My Role
My role is to provide conservative treatment options to patients with back and neck pain. I also accurately diagnose painful spinal conditions and move the patient through a thorough treatment process. This begins with the least invasive options, and if the patient’s pain doesn’t improve then we determine if surgery is necessary. Ultimately, my role is to ensure a patient’s source of pain is accurately identified and treated.
My Goal
I bring the most current and minimally invasive treatment options for spinal pain to the Black Hills. Nobody wants pain and discomfort to limit what they can do, and I want to help patients get relief. Hopefully that allows them to return to activities and lifestyles that they enjoy. My goal is to help each patient live their best life and contribute to better spinal health throughout the region.
My Passion
The most rewarding part of my job is seeing patients improve their quality of life and regain the ability to do the things they love. Outside of work, I’m Passionate about my children — anything I do with them! We love exploring the Black Hills and spending time in the outdoors, kayaking, canoeing and camping. I am also very grateful for the friends I have made in the time that I have been here.
My Role
I have been with Monument Health for 23 years, and my current role as Valet Supervisor is to help ensure patients’ cars are safely parked at Rapid City Hospital. Many patients tell us getting to and from their appointments would be much more challenging without this service. It’s especially helpful during the cold winter months.
My Goal
At the end of the day, if I can help a patient feel like a VIP, I have achieved my goal. I hope I can put a smile on everyone’s face who I come in contact with, and hopefully that will set a standard for the rest of their visit. My team and I are very dedicated to creating a positive experience for patients.
My Passion
At the end of the day, I feel good knowing I was part of caring for our patients and their families. Outside of work, I enjoy camping and taking our Jeep throughout the Black Hills. My wife and I just became first-time grandparents; I’m looking forward to this new adventure.
For many, the valet is the first and last caregiver a patient will see during their visit to Rapid City Hospital. Their kindness and customer service can help set the tone for the patient visit. On an average month, Valet Services park and retrieve 2,800 cars and help welcome 2,100 patients — this includes assisting with wheelchairs when necessary.
“I made the decision to stop playing basketball and tried to focus on what I was going to do for a career,” he said. “I started volunteering in an emergency room (ER) and got an up-close introduction to nursing. Once I made my decision, I finished my prerequisites and applied to nursing school and got in.” With that, he began his career in nursing.
From his time volunteering, James knew he wanted to work in an emergency room. “The intensity of the ER is what drew me to it. There is always something different coming through the door. It’s always changing, and it keeps you on your toes,” James said. “You have to be ready for anything, and that really drew me to it. I wanted to be a nurse first, but I knew I wanted to work in the ER. You get to save lives on a daily basis.”
After graduation, James worked at two different health care organizations in Arizona: Banner Health and Tenet Healthcare. He said both felt too big for him. James wanted to work somewhere patients were treated like people — ideally small-town medicine, but with the skills and expertise found in metropolitan hospitals. “I was looking for an organization that was not quite as large, but still had their stuff together. I wanted to work for a system that was smaller, but still established.”

Rural Life
James was on the lookout for a health care system that he fit into, and South Dakota was on the short list. James said, “My wife and I wanted to be in the Black Hills area. We were open to anywhere from Spearfish all the way down to Hot Springs. I had been keeping my eyes open for an opening here for probably a year-and-a-half, but I was really picky.” He had family in the area and was drawn by the beauty of the hills, but he was also looking for the right hospital to make his home.
It only took one interview with Monument Health Custer Hospital for James to know this is where he wanted to expand his career and create a life. “There truly is a family atmosphere. You get to know most of your patients on a personal level, you see them around town, there’s a high level of accountability among everyone here. Everyone truly goes above and beyond to make it a better place for both the patient and for the people who come to work here.”
The community of Custer and Monument Health leadership have invested in the health of the Southern Hills community — that impact was evident to James. Monument Health and the City of Custer partnered to build the $22 million hospital and clinic, which opened in May 2018. It includes inpatient rooms, clinic care, physical therapy, urgent care services, an emergency department and a healing garden.
“It was clear to see how far along the Custer Hospital was. I could see the dedication to providing the best care to their community. Custer has a lot of resources and an organizational structure that you don’t expect to see in a lot of other critical access hospitals. It strikes the balance between that small town atmosphere with the level of care that comes with a bigger hospital,” James said.

Advice for the next generation of nurses
James has found success in the health care field, and his leadership has helped Monument Health become a great place to work. He said one of the keys to success in nursing is being open to feedback. “Always be open to whatever feedback someone is giving you. Even if you’ve heard the same thing several times before, just listen to what that person is saying,” James said. “It builds trust, and they could always give you new information or present it in a new light.”
He also stressed that nursing students shouldn’t get too buried in books. “Really listen to your instructors, especially when you’re in your clinicals, and be more aware of your surroundings.” He stressed that while there is good information in written materials, real-world nursing is dynamic, and instructors will have insights on how to solve problems. James also said it’s important to work on your people skills because nursing is very people-centered. “You either have to be a people person or be willing to work on and build that skill,” he said.
James emphasized the importance of work-life balance in nursing. “It’s a high-stress career. There’s a lot of pressure put on everybody’s shoulders to get a lot done in a small amount of time. I cannot stress enough, people in the profession need to find balance in their lives. If they don’t take care of themselves, they’re not going to do a good job taking care of other people.”
“I would also recommend finding the right place for you,” James added. “You will grow and flourish when you find where you belong. That’s what Custer has done for me. There’s no place better, as far as I’m concerned.”
Written by David Scott
Photography by Bob Slocum
When Deb Fredrich first began to investigate hospice care, she just
wanted to understand it. Perhaps she was looking to heal a piece of herself and didn’t intend to get wrapped up in it. When she reached out to her local hospice care center, hoping to understand more about death and dying, they offered some educational opportunities which proved more consequential than she first imagined. Eventually, she was asked if she would consider volunteering in the home to work with patients and their families.
“At first I didn’t want to volunteer in hospice, because I knew I couldn’t keep people from dying,” Deb said. “Then I was told they wanted me to visit a baby.”
One leap of faith later, she found herself entering a stranger’s home to visit the child. Her trepidation in the unfamiliar situation melted away once the little one was in her arms. “This baby was two months old, and I began to visit the family every third day,” she said. “The child was dying of brain cancer, and I asked what I should do. They said, ‘just hold him.’ They just wanted him to be held. It just totally pulled me in. It was totally a God thing, otherwise I would have never volunteered.”
A former Monument Health Auxiliary president, Deb recently received her recognition pin for 10,000 volunteer hours. Along the way, Deb has picked up much more than mere acquaintances and incidental memories. Some of the bonds formed along the way have endured and new friends have become like family. Deb says her time with patients isn’t always somber, in fact it’s often quite the opposite.
“I’ve met so many good people. That’s the fun part. With hospice care, I’m not helping them die, I’m helping them live. There is a patient I have now, we just make each other laugh the entire time.”

Deb Fredrich was gifted this “circle of children” keepsake to symbolize all the lives she’s touched as an in-home hospice volunteer who often visits sick children.
She also has amassed more than 10,000 hours volunteering at Monument Health in various roles, but primarily as an in-home hospice worker. She is also a former president of the Volunteer Auxiliary. The ornamental pin she wears was a gift meant to represent all the lives she has touched in her volunteer career.
Often, in-home hospice patients have family by their side, who may receive a break when help arrives. Hospice care in the home is something many in the position desire, but it can be taxing on the family.
“It’s someone else to visit with, someone else to lend a hand. You’re there for the caretakers, too … the husband or the sibling, because they are there all day.”
Aside from providing a reprieve to those sitting vigil for the patient, Deb said a third party from outside the family can sometimes lift spirits or ease tension by precluding the stigmas around death and hospice.
“A lot of times when you’re dying, people don’t know what to do or what to say. People can get lonely. It’s not about fixing it; it’s about not shying away from it. They may want someone to cry with, or laugh with, but it’s just about empathy. My sister died at age 9 when she was home so in a way, I think that’s where it started, because at that time people were there for us. One patient’s husband asked me, ‘why do you do this?’ And I said, ‘well, somebody did it for me.’”

Although she has worked in the home and also at Monument Health’s Hospice House, Deb has volunteered in other areas.
“I started there and then I volunteered in one of the areas where we connect doctors with the families of patients who are in surgery. In that role, you do a lot of listening. You’re part of the support system. I did that for a few years and now I’m going to the gift shop once per week. The gift shop really is like a ministry in a way. People just want to talk. Everyone has a story and wants their story to be heard.”
Ten thousand hours is a long time to spend doing anything, but to spend it in service to others is a unique undertaking. Ten thousand hours is a long time to spend doing anything, but to spend it in service to others is a unique undertaking. It’s often said that 10,000 hours is the amount of time needed to master a skill. If so, Deb has truly mastered the art of compassion. She said her experience over the years has been ultimately uplifting and restorative.
Volunteers play a vital role in providing a caring experience for our patients and families. If you have a passion for helping others, consider becoming a volunteer. “I always tell people they are part of a legacy of volunteers,” said Konnie Sorenson, Volunteer Services Manager for Rapid City Hospital. “Even before Rapid City Hospital was formed, there was a precedent for community members coming together to aid those in need. We’ve got some awesome people who volunteer with us and keep that tradition alive.” For more information about volunteering or to learn how to get involved, visit monument.health/volunteer or call Volunteer Services at 605-755-8980.
“I’ll probably do this forever,” she said. “Gratitude is a big one. We’re grateful. My family has been so blessed and it’s nice to give back. I feel like we make a difference but mostly they make a difference in me. It has helped me to listen more attentively. Each situation is different, and I don’t want to have an agenda. I go in hoping to provide whatever they need. One family had a sick baby and the mother was also home with two preschoolers. I ended up being godmother to the family’s next child, and I first came into their home as a stranger. It’s not really me, it’s the Holy Spirit, it’s God working through me.”
Written by Bob Slocum
Photography by Bob Slocum
Where do you volunteer, and what are your duties?
My main duty is to escort patients to different areas of the hospital. Some of the areas are MRI, surgery waiting room, Respiratory Therapy and Heart and Vascular. We deliver flowers to the patient rooms. Many of the visitors who come in do not know how to get to patient rooms, and we escort them to the elevator, the ICU or to pediatrics and obstetrics, among other areas.
Why do you volunteer?
Because I am retired and enjoy keeping busy. I like helping people, and it enriches my life. People are very thankful for what we do.
For more information about volunteering or to learn how to get involved, visit monument.health/volunteer or call Volunteer Services at 605-755-8980.

What is your favorite part of volunteering?
I enjoy talking with people and making them feel welcome and comfortable when they come in for an appointment or as a visitor. I work with great people who I would never have met outside of volunteering.
Would you recommend volunteering to others?
I tell people that it is a good way to give back to the community and it is a fulfilling, enjoyable experience.
Why is Monument Health a good place to volunteer?
I think volunteers benefit from Monument Health in knowing we are doing something to help someone else. We receive nice perks, like coffee, lunch and coupons from the gift shop for our birthdays. Also, a benefit for me is that I try to walk at least 10,000 steps a day. I can almost get that many during a 4-hour shift, which is why I am always eager to escort patients and visitors wherever they need to go. The busier we are, the more I like it!
What is asthma?
Loren Jones, M.D.: Asthma is an inflammatory disease in the lungs that impacts the small airways or bronchioles. Inflammation of these airways causes them to narrow. It can also cause spasms of smooth muscle in the walls of these airways, which squeezes them and narrows them further. This can cause acute asthma attack symptoms like shortness of breath, cough and wheezing.
What are allergies?
V. Richard Bowen, M.D.: In people with allergies, the immune system identifies allergens — like pollen or certain foods — as dangerous, even though they’re not actually harmful. The result is inflammation of the skin, the sinuses, airways or digestive system. For some people this leads to minor irritation, but for others it can cause life-threatening responses.
Loren Jones, M.D. is an Otolaryngologist (ear, nose and throat physician) at Monument Health in Spearfish with more than 13 years of experience. He is a Fellow of the American Academy of Otolaryngology-Head and Neck Surgery. Dr. Jones diagnoses and treats the full spectrum of ENT conditions, specializing in minimally invasive and office-based sinusitis treatments.
How common are asthma and allergies?
Bowen: They are fairly common. Allergic rhinitis, or inflammation of the nose, affects 10 to 30 percent of the population. Some estimates suggest that asthma affects 300 million people worldwide. Roughly 80 percent of asthmatics also suffer from allergies.
Can allergies affect asthma?
Jones: Allergies can certainly affect asthmatics. The linings of the nose, throat, sinuses and lungs are all the same type of mucus membrane tissue and are largely susceptible to similar problems. In the same way that allergens can trigger the immune system to produce inflamed nasal tissues, they can also affect the airways of the lungs. In fact, some medications are used to treat both allergies and asthma.
Do men and women have different rates of asthma?
Bowen: Childhood asthma is more common in boys than girls — by a 3-2 ratio. However, this changes as we age: there are more women than men with asthma as adults, with eight women with asthma for every two men.
 V. Richard Bowen, M.D. is an Otolaryngologist (ear, nose and throat physician) at Monument Health in Rapid City with more than 20 years of experience. He is a Fellow of the American Academy of Otolaryngology-Head and Neck Surgery, a Fellow of the American Academy of Otolaryngic Allergy (AAOA) and a Diplomat of the American Academy of Aesthetic Medicine.
V. Richard Bowen, M.D. is an Otolaryngologist (ear, nose and throat physician) at Monument Health in Rapid City with more than 20 years of experience. He is a Fellow of the American Academy of Otolaryngology-Head and Neck Surgery, a Fellow of the American Academy of Otolaryngic Allergy (AAOA) and a Diplomat of the American Academy of Aesthetic Medicine.
What is the most common type of allergy?
Jones: The most common type of allergy is pollen. This can be from trees, weeds and grasses. Allergic reactions to pollen are often referred to as hay fever. Other common triggers include pet dander, molds, dust mites and cockroaches — fortunately we don’t have to deal with cockroaches much in our area. The most common food allergies depend upon age. In children, milk, eggs and peanuts are the most common. In adults, the most common food allergen is shellfish.
Is there anything about western South Dakota that makes allergies and asthma more of a concern?
Bowen: The most problematic allergens, like pollen, are those that travel the furthest in the wind. That means individuals with allergies or asthma may have a problem in windy areas like western South Dakota.
Can allergies develop at any age?
Bowen: Allergies may develop at any age, but it’s most likely through the teens and early 20s. Infant allergies are usually food related or manifest in skin conditions such as eczema. When allergies first occur later in life, it is often because a person is exposed to allergens when their immune system function is compromised — such as when they’re sick or pregnant — or when they are exposed to new allergens.
Are people more likely to have multiple allergies or just one?
Jones: Yes, if you have one allergy, it is more likely you will have others. It’s unusual to test positive to only one allergen, although not unheard of. Since allergies are a function of a misguided immune response, the fact you have one allergy indicates that the immune system may be more likely to develop allergies to other things.
Do allergies ever go away?
Bowen: The good news is, yes, the older we get the less severe allergy symptoms become. Unfortunately, this may not occur until after age 60 for many people. However, for most folks, allergies greatly improve with test-specific allergy shots, or an under-the-tongue therapy. We recommend four to five years of therapy, that may give eight to 10 years — or more — of symptom relief.
Monument Health now provides Ear, Nose and Throat (ENT) services in Rapid City in addition to ENT services in Spearfish. To learn more, visit www.monument.health/ent.
My Role
I am privileged to partner with caregivers and providers from all specialties across our system to help communicate any emergencies and work through any process improvement opportunities. My teams are part of Safety Services, which means when an emergency call comes in, all other calls go on hold.
My Goal
To provide support to our community, patients and caregivers through compassion. Our willingness to relieve the suffering of others builds trust with each other and our community. We do that by listening and taking appropriate action to get them the help needed. Most people who call the hospital are looking for help; my goal is to live up to that basic expectation.
My Passion
My passion is being prepared for emergency situations and knowing our hospitals are prepared. I love the partnership between so many departments to help support their communication needs when it’s most important. I enjoy being part of something with such a huge impact, yet totally behind the scenes. The heart of everything we do is for the people we serve.
The Communications Center caregivers answer around 33,000 calls per month — this includes about 4,600 emergency calls. Emergencies include paging physicians and caregivers if a patient is having an emergency, when critical tests results are ready, if security is needed or if there is a natural disaster. The Communications Center responds to emergency situations to ensure they are communicated to the proper teams, such as a Rapid Response or Fire.
 Joseph Tuma, M.D., FACC, FSCAI, Interventional Cardiologist
Joseph Tuma, M.D., FACC, FSCAI, Interventional Cardiologist
I have two rules for procedures, no country and no Christmas music! Usually I enjoy listening to 90s rap — Snoop Dogg, Tupac, etc.
 Ray Jensen, D.O., Orthopedic Surgeon
Ray Jensen, D.O., Orthopedic Surgeon
Typically, I listen to classic or alternative rock. My favorites are Mumford and Sons and the Lumineers.
 Alice Police, M.D., FACS, Breast Surgeon
Alice Police, M.D., FACS, Breast Surgeon
In the OR, I listen to whatever the hardworking nurses want to hear. They are so wonderful and I always let them pick, even if it is country music, which I dislike intensely.
Kyle Schmidt, M.D., Neurosurgeon
I prefer country music, old or new, I’m flexible. If it is a long case then I do Avicii Radio.
 Richard Little, M.D., Orthopedic Surgeon
Richard Little, M.D., Orthopedic Surgeon
Simple. For me, it’s classic rock.
 Saverio Barbera, M.D., FACC, FHRS, Cardiac Electrophysiologist
Saverio Barbera, M.D., FACC, FHRS, Cardiac Electrophysiologist
We listen to a little bit of everything! Mostly it’s going to be classic 70s rock or classic country. Sometimes we’ll throw in a little jazz or Frank Sinatra. Everybody gets a chance to pick the genre for the procedure. I really believe that listening to music enhances the experience overall. It improves mood and concentration.
 Michelle Krohn, D.O., OB/GYN
Michelle Krohn, D.O., OB/GYN
We go around the room and let everybody have a chance to pick what we’re listening to — sort of like MTV’s Total Request Live!
 Rachel Michael, M.D., Orthopedic Surgeon
Rachel Michael, M.D., Orthopedic Surgeon
My playlist includes about 60 hours of music from all genres. We put it on shuffle for everyone in the OR to enjoy. This way, if someone doesn’t like a song, a new option in a new genre comes on in just a few minutes. It covers rock, rap, hip hop, international, broadway musical, classical, indie, Disney, top hits, country, metal, punk, Latin, blues, R&B, folk, jazz, EDM, disco, 1920s-2022 music... You name it, it’s on there. It helps keep everyone happy and allows for a fun day while we are all working hard for our patients.
My playlist is public on Spotify, give it a listen! Just search OR Tunes.
 Dan Lochmann, M.D., Orthopedic Surgeon
Dan Lochmann, M.D., Orthopedic Surgeon
When I’m in the OR, I’m usually listening to 80s and 90s rock. My favorite, though, are the Rolling Stones.
 Katherine Croft, M.D., Gynecologic Oncologist
Katherine Croft, M.D., Gynecologic Oncologist
I don’t have a surgical playlist because we usually listen to Pandora in the operating room. When I was a trainee, the first thing I wanted to do as an attending was to get to play Metallica in my OR! Once this happened, I settled into classic rock, which is my go-to. In general, anything with an electric guitar makes me a pretty happy camper. I also listen to 90s alternative rock/grunge, 80s hair metal and 90s Hip Hop. I don’t think you can ever go wrong with a little Taylor Swift or Lizzo.
I listen to music that makes me happy and blends into the background while I am focusing on the surgery. I grew up listening to all of these songs, and peaceful background music keeps me calm in stressful situations that occasionally arise.
 Bradley Anderson, M.D., FACS, Urologist
Bradley Anderson, M.D., FACS, Urologist
I have created two playlists for when I’m in the OR. I always let the scrub tech choose which one we’re going to listen to. The first, “Brad’s Killer Country” on Spotify. It’s 49 hours long. Or we go with my other Spotify playlist, “Brad’s Shamelessly Clichéd Pop,” which is 44 hours long. When those are on shuffle you hear something new each surgery. Both lists do have one thing in common, they are exclusively upbeat.
As much of the world becomes more convenient and more automated, so has medicine. Online companies like Amazon Pharmacy, For Hims, For Hers and others have expanded the ways people can have their prescriptions filled.
Dana Darger, RPh, is Director of Pharmacy at Monument Health Rapid City Hospital. He said that there’s nothing inherently wrong or dangerous with these online pharmacies. He is leary, however, of some of the motivations behind using these ultra-convenient pharmacies.
“It’s hard to say if getting your medications prescribed and filled online is safe or not,” he said. “But, some of it can be a bad health care paradigm.” Dana explained that providers are best able to help patients improve their health and wellness when they are working with a complete health care picture.
For instance, a common prescription drug that patients seek online is sildenafil, a treatment for erectile dysfunction. Some sites like For Hims allow patients to get prescriptions like this generic version of Viagra after filling out an online form and having a brief consultation with a doctor online or over the phone.
“If you get an online prescription and if you aren’t paying through insurance, there’s no record of you taking this drug,” Dana explained. Prescription records are kept in tandem with insurance in most cases. So, the only way a provider might know that a patient who paid for sildenafil with cash is taking the drug would be if the patient volunteered that information — something that might not happen. Sildenafil interacts with certain heart medications, and if providers don’t have that drug in a patient’s records, and the patient doesn’t disclose that information, the results could be disastrous.
“The other issue might be that people are assuming that ED is only a symptom of aging,” Dana said. “There actually could be a lot of different health conditions that could be causing that — serious ones.” Seeking out automation and convenience is only natural. Dana’s advice is not to shortchange your own health care. He said to make the time and cultivate that relationship with your pharmacist and other providers. An online pharmacy, if used responsibly, can be a great tool. But nothing can replace a capable provider with a full picture of your health care needs.
Online pharmacies and other telehealth services are the future. The FDA has released a guide to navigating online pharmacies safely.
Safe Signs
Your online pharmacy is likely safe if it:
• Always requires a doctor’s prescription
• Provides a physical address and telephone number in the United States
• Has a licensed pharmacist on staff to answer your questions
• Is licensed with a state board of pharmacy
Warning Signs
Your online pharmacy may be an unsafe website if it:
• Does not require a doctor’s prescription
• Is not licensed in the United States and by your state board of pharmacy
• Does not have a licensed pharmacist on staff to answer your questions
• Sends medicine that looks different than what you receive at your local pharmacy
• The medication arrives in packaging that is broken, damaged, in a foreign language, has no expiration date or is expired
• Offers deep discounts or prices that seem too good to be true
Written by Stephen Simpson
Why do you volunteer with Monument Health?
I spent essentially all of my adult life working in a hospital, and I love that environment. I love working with hospital personnel, particularly the nursing staff and the nurse aides. This gives me an opportunity to do what I love and to help out the nurses that are volunteering at the same time.
What is the Volunteer Nurse Corps?
In South Dakota, nurses must actively work in nursing to renew their license. They have to get a certain number of hours in each two year cycle, and if they don’t want a job — perhaps they are retired, or a stay at home parent — but want to maintain their license, they look for opportunities to work in nursing as a volunteer. When I came to volunteer in 2013, I was asked to take over the program and make sure it was working properly.

What else have you done as a volunteer?
I’m very proud of my role in starting Operation Patriot. I am a retired military nurse and when I started volunteering I wanted to find a way to show veteran patients that the hospital cares about them. We came up with certificates to show appreciation, and then pins were added. We started with me going around and giving veterans their pins and certificates, but I was only there once a week. Since then, the Monument Health Military Veterans Group has taken over and they have done an excellent job.
What advice do you have for anyone who wants to volunteer?
Come on over! There are so many ways to help. Whether it’s as a nurse or a wayfinder, we’ve got a place for you and could use your help.
Why do you volunteer?
After semi-retiring from ranching in Perkins County, I was looking for an opportunity to meet people and get involved in the community. I was invited to join the hospital auxiliary and joined in 2013. I started volunteering in the gift shop because I had seen how nice it was, and I thought it would be a fun thing to do.
How did you end up managing the gift shop?
The lady who was running it asked me to take it over as she said she was running short on time to keep it up. I thought about it for a while and decided to go for it. That was in 2016. It has really been fulfilling, and I’ve really enjoyed it.
What is your favorite part of volunteering?
I enjoy seeing all the customers, especially as many of them are Monument Health caregivers.
I also enjoy stocking the store and having different items available for people.

How does the Sturgis gift shop benefit Monument Health?
Our funds have been used for scholarships, we’ve helped remodel a room in the nursing home as well as the beauty shop and we donate to other community interests outside Monument Health as well. The purpose of the gift shop is for local fundraising.
Why do you think it’s important to give back to your community?
It keeps the community together. It helps those in need and helps promote Monument Health, which is great, because Monument Health is so important to our communities when you look at how many people it serves and all the services it offers.
Sandra Gruenig, Registered Nurse and Clinical Coordinator at Rapid City Hospital, didn’t plan to enter the nursing profession. Sandra originally completed her degree in engineering while she was living in her home country of the Philippines. As it often does, life sent her in an unexpected direction. She married an American citizen and moved to the United States, where she wasn’t able to find work in her field. While working in an assisted living facility she began to consider returning to school to become a nurse.
If you had asked her earlier what profession she’d choose, nursing would have been one of her last answers. She had a lot of misconceptions about the profession that changed when she started the program. “I used to think of nurses as just the doctor’s assistant, but it’s much more than that. You really are a team,” Sandra said. “You’re the doctor’s eyes and ears when they aren’t there, and nurses are the people who spend the most time caring for patients.”

RETURNING TO SCHOOL
Sandra was accepted to the South Dakota State University School of Nursing in Rapid City. She said it was a challenge to overcome some obstacles. “In the Philippines, most of our classes are taught in English by the first grade, so when I got here I knew how to speak English,” she said. “But it was intimidating, at first, to try and express myself. I felt like it took twice the effort just to comprehend all the information I was getting, or sometimes my coworkers would make a joke and I wouldn’t really understand it.”
Sandra was able to use her experiences to help a group of new Filipino nurses at Monument Health adjust to new equipment and processes they weren’t used to. “They were having a hard time with things like using infusion pumps to measure flow rates. They would tell me they didn’t really use those. They were used to calculating flow rates manually.”
Helping and working with those nurses provided a new lens for her and other managers to look through. “Understanding the training people received, and how they approach things differently, helped us understand what to expect and taught us how to prepare new nurses who were trained in other countries.”
EXPLORING HER NEW CAREER
Sandra joined Monument Health directly out of school but wanted to understand how other health care systems operated. She spent half a year working as a traveling nurse with the University of Nebraska Medical Center, and she credits Monument Health for supporting her traveling and exploring what opportunities were available. “I did not really leave Monument Health, but I stayed a PRN for a time and I went traveling,” she said. “I planned to come back, but I also wanted new experiences and wanted to know what’s out there, probably for my own satisfaction, and they were really supportive of that plan.” PRN is taken from the latin pro re nata, which means “as the situation demands” or “as needed.” PRN nurses do not work full time but rather work as needed and as their schedule allows.
She said culture shock isn’t only for people coming from other countries. “It’s not just the difference between the United States and the Philippines. When I went to Nebraska, their culture was very different.” Everything, from the way doctors and nurses interacted to how they did things changed significantly from what she was used to. “When I got back to Monument Health and people were talking about being short staffed, I was like, ‘You think we’re short staffed? This is not short staffed.’”
LOOKING BEYOND PASSION
Sandra said Monument Health has become a more supportive organization over time because the health care system has faced and adapted to many challenges, particularly regarding training and preparing caregivers who come from other health care systems. She said experienced managers go a long way in helping people feel at home. “I think managers have a better idea about what to expect and what challenges there are. We’ve learned the questions to ask to find out what new nurses need when they come in from other organizations.”
Sandra encourages people who want to get into nursing to understand what is motivating them to do that. “When you ask somebody why they want to be a nurse I feel like many people would say, ‘Oh, because I’m passionate. I want to do this job.’ Passion is an important part, but nursing is a lot of work and requires a lot of patience, and they need to think about if that is something they want.”
She noted the importance of being able to see the patients as people and feels like that can be easily overlooked. “That patient is also a mother, a sister, a brother or someone else important to another person. Ask yourself, if it was your family, how would you want them to be treated, then work to give every patient that level of care.” Sandra’s patience and dedication to her patients has been a constant over her career. In 2021, she received a daisy award after a patient nominated her for her compassion and care.
Benefits of having international nurses
Foreign-born professionals make up a sizable group of the nation’s health care workforce. More than 2 million health care workers in the United States immigrated from other countries, and physicians and registered nurses represent more than half that number. Our nation’s health care system relies on the expertise and perspectives of foreign-born health care professionals to function. Immigrants make up a larger portion of the health care field than they proportionally do for other sectors. Diverse perspectives help us to improve the quality of the care we can offer to the communities we serve. Whether they received their education outside the United States or started on a new path after arriving, the health care professionals who immigrated here are invaluable, not only to our health care system, but to the communities in which they live.
-Nicole Kerkenbush, Chief Nursing and Performance Officer

What is a DAISY?
Monument Health recognizes the hard work of nurses and their support teams through two different awards, the DAISY and TULIP.
The DAISY Award is a nationwide program presented in collaboration with The American Organization of Nurse Executives (AONE) that rewards and celebrates the extraordinary clinical skill and compassionate care given by nurses every day. It was established by the DAISY Foundation in California in memory of J. Patrick Barnes, who died at age 33 of an autoimmune disease. DAISY is an acronym for “diseases attacking the immune system.” Nurses can be recognized by patients or by the patient’s family, and other caregivers for their outstanding service.
TULIP is an acronym for, “Thoughtful upbeat loving individuals caring for patients,” and the TULIP Award recognizes outstanding members of Monument Health’s nursing support teams. Nursing support includes positions such as Nurse Aides, Certified Nursing Assistants, Emergency Department Technicians, Psychiatric Technicians, Health Unit Clerks, Dialysis Technicians, Clinical Assistants, Cardiac Monitoring Technicians, Activities Assistants, Medical Assistants, Certified Medical Assistants, Medication Aides and Restorative Assistants. The TULIP award is specific to Monument Health.
Twelve nurses and nursing support caregivers in Rapid City are selected for each of these recognitions each year. They are also honored in Custer, Lead-Deadwood, Spearfish and Sturgis.
Written by David Scott Photos by Robert Slocum
My Role
I am currently in the Human Resources Department as an HR Business Partner, supporting the Northern Hills Market. This includes all hospitals and clinics in the Lead-Deadwood, Sturgis, Spearfish and Belle Fourche communities. As an HR Business Partner, I provide consultation and support to our leaders and caregivers on all HR matters ranging from employee relations, staffing needs, policy interpretation, coaching, performance management and many more.
My Goal
I strive to bring a positive energy to our Northern Hills locations for both leaders and caregivers. Every day I ensure that I am a trusted partner for our teams, whatever the issue may be. My goal is to aid the organization by supporting leadership strategically and to help our caregivers through all situations relating to Human Resources. I take pride in responding to and getting answers out in a timely manner. If I don’t have an in-depth answer to a caregiver’s question, I am proud to be part of a phenomenal team of HR professionals who also provide their input and support to ensure we are meeting our client’s needs.
My Passion
My passion is driven by knowing the work I do strategically supports our leaders and caregivers so they can provide the best care to our patients. I think a lot of people view human resources as a tough role, but I view it as a way to ensure Monument Health is a great workplace for our caregivers, who are our most valuable asset. I believe strongly in upholding and supporting Monument Health’s mission, vision and values so we can collectively grow together in the same direction and strive toward the same goals.

Monument Health’s human resources teams deal with everything worker related. This includes talent acquisition, training and development, promoting and onboarding, as well as dealing with employee health, morale and engagement.
Other teams and departments that fall under the human resources umbrella include the Total Rewards program (which deals with caregiver benefits and compensation), Enterprise Resource Planning, the System Workforce Service Center and Child Care. The total department is comprised of more than 65 caregivers across the system.
Zombies exist purely in the realm of science fiction, but, as many parents and guardians of teenagers know, something vaguely reminiscent of the horror movie staple can often be seen stumbling to the breakfast table — or straight out the door — on any given morning. “Most kids are just not getting enough sleep,” explained Eric Santure. He works with athletes at Spearfish High School
and is a Performance Enhancement Specialist with Monument Health Orthopedics and Sports Medicine.
And it’s not just a full night’s sleep that teens are missing. Eric and his sports medicine colleagues at Monument Health work with high school students every day, and they see both the chronic undersleeping and undereating that is afflicting teens. They also know what it takes to get teenagers out of the fog and back to their best.
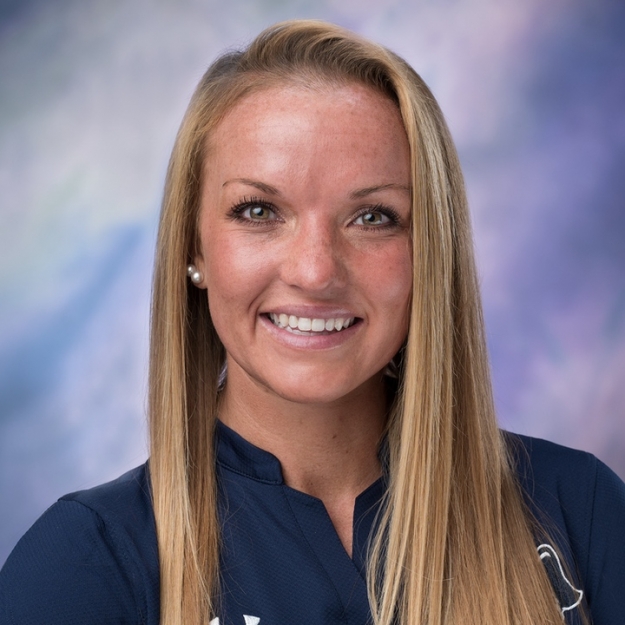
Off to Never-Never Land
Faith Wilson, Performance Coach for Monument Health Sports Performance Institute and South Dakota Mines, explained that there’s a lot at stake when it comes to teens getting adequate sleep. “It’s been proven when sleep quality decreases, so does attention span in school,” she said. “Mental health is impacted. Performance and recovery as an athlete declines. The likelihood of injuries while playing sports goes up, too.” Almost every aspect of a teen’s life is impacted in a negative way by scant slumber.
Eric said that a common early morning scene at the Spearfish High School gym is under-fed and under-rested teens. “Their faces turn pale, and they’ll look absolutely exhausted after about five minutes of weight training. And then I’ll ask them what they did last night; it’s usually something like, ‘played Xbox until 1 in the morning.’”
Running on Empty
Eric’s follow-up question to his lethargic lifters usually centers around their food intake that day. The typical breakfast? “Nothing,” Eric reported. “The large majority of high schoolers are chronically undereating,” he said. “Chronic undereating in teenagers impacts their attention span in the classroom. And it impacts their performance and recovery as an athlete.”
Faith said, “Most teens I know — and most people in general — don’t want to go into exercise feeling full. But you need to have something in your stomach — a piece of toast or half a Clif Bar or something. Running on empty while working out has the potential to cause some major damage.”
Food as fuel is a mantra that can be heard consistently from Monument Health’s sports medicine caregivers. And for athletes, this metaphor is obvious — if you want your body to perform in a certain way, then it needs access to carefully curated nutrition — and a lot of it. But what about those moments when your teen’s body doesn’t need to bench 200 pounds or sprint up and down a basketball court for 48 minutes? Does a teen body still need the kind of beefed up calorie consideration that these coaches are preaching to their athletes?
The average teenager burns more calories than the average adult. For most teens, their bodies are still growing. These growth spurts require a huge uptick in caloric intake. But teens aren’t just growing physically. They also need to consider mental performance.
Always on My Mind
Teens are burning calories in calculus class. A teen’s brain needs fuel just like the rest of their body. The biggest fuel source for a teen’s brain — or anyone’s — is a nutrient that has gotten a bit of bad rap. Alissa Towsley, Performance Dietitian at Monument Health Sports Performance Institute, reveals the brain’s preferred fuel: carbs.
Carbohydrates, despite being dragged through the mud in recent years, are a vital source of energy for the human brain. “It’s all about nutrient timing and knowing the different kinds of carbs out there,” Alissa said. “Simple carbs are like white bread, pasta and some kinds of fruits — our bodies can easily and quickly utilize these to refuel, so simple carbs are good for a quick burst of energy.” Feeling sluggish and you have that history exam in 10 minutes? A PB&J might just provide your teen with enough perk to get through those essay questions with a clear head.
What about that day of back-to-back finals? Start your morning with carbs of a different variety. Alissa explained, “Complex carbs are things like whole grains and oatmeal — things with fiber in them. Complex carbs will help you feel fuller longer and help with digestion.” Steady, consistent energy through the day is what complex carbs are bringing to the table. Learning to time carbs is key to staying alert and running at full capacity, both at practice and in class.
Hydrate
Alissa Towsley, Performance Dietitian for Monument Health Sports Performance Institute, said, “Drink half your body weight in fluid ounces. So, for a 150 pound individual, they need to be drinking 75 fluid ounces; 20 ounces for every hour of exercise. If it’s hot, replenish electrolytes.”
Electrolytes are salts that living things use to maintain healthy body systems. Humans and other animals need electrolytes for things like muscle contractions, to maintain proper blood pressure and other vital functions. “Hydrate right away in the morning,” Eric added. “You don’t want to play catch up with hydration. Drink a big glass of water with your breakfast, not just coffee.”
All in All
So how do we keep our teens well-fed and playing and learning at their best? Alissa said that routine is a big factor for feeding teens well. “Having a consistent eating schedule is huge, including regular snacks.” Make breakfast quick and predictable and something that is enjoyable to eat. Make it something hard to skip.
And make snacks readily available. Chips and cookies have their places, but access to nuts and other foods with plant-based fats have special benefits. “Unsaturated fats — found in things like nuts, olive oil and other plant-based fat sources — help with cell structure and can reduce inflammation. They can also help with mental clarity,” Alissa said. She added that crafting meals can be simple if you remember the three-for-three rule. “That means three meals a day with these three things: a protein, a carb and a fruit or vegetable.”
Putting all of these feeding instructions together may seem a little bit like looking after a gremlin, but making sure your teen is rested and fed enough couldn’t be more crucial to their success in both sports and in the classroom. Food is fuel, after all.
Carbohydrates
Has there ever been a more notorious nutrient? Carbs are a hotly debated topic for many dieters. Should this macronutrient get such a bad rap? Probably not, said Alissa Towsley, Performance Dietician for Monument Health Sports Performance Institute. “It’s our brain’s preferred energy source,” she said. And she explained that carbs come in two varieties: simple and complex.
“Simple carbs are great for a quick burst of energy. Complex carbs can give us a longer, more consistent source of energy.”
Simple carbs include:
• Milk
• Cookies
• Bananas
Complex carbs include:
• Whole grains
• Apples
• Beans

Protein
Working out without any protein is like having a crew show up to construct your house without building materials.
“If we have protein readily available in our bodies after a workout — from a protein shake or some chocolate milk — we’re guaranteeing that there’s a big stack of lumber and a big bucket of nails ready when the carpenters show up,” Eric said.
Did he say chocolate milk? Over 20 papers have been published that support drinking chocolate milk post workout. As a liquid, it’s quickly consumed and digested. And the protein to carbohydrate ratio in the beloved beverage is just about perfect for most people. “There are a lot of Division 1 universities that stock their weight room coolers with chocolate milk,” Eric added.
Written by Stephen Simpson
Put simply, health care in this region is better because of Julie Raymond, M.D. Her work, particularly in breast health, elevated the level of care that is available to the people of the Black Hills. But it wasn’t just her work that inspired her colleagues to strive for excellence. Her life was a study in human compassion. “A legacy of love,” Alice Police, M.D., labeled it.
Dr. Police came to Monument Health with surgery experience from hospitals in New York and California. She expected to bring the cutting edge procedures and protocols of these big city hospitals to Rapid City.
“When I came here, I expected to find a rudimentary breast care program. I was blown away by the program I found,” she explained. Dr. Raymond laid the foundations of an astonishing breast care program at Monument Health. “There are some breast care programs in New York and California that aren’t as sophisticated as the one here,” Dr. Police shared.

The Dr. Julie Raymond Memorial Fund honors Dr. Raymond’s dedication to breast health education in the community. Funds raised support the continuation of her vision and passion through community education and events. Donations can be made by visiting monument.health/donate.
How good she was
It’s one thing to provide outstanding care. It’s something entirely different to provide excellent care that is warm and caring at its roots. Dr. Raymond’s heart was always aimed at helping people. “She was the most compassionate person I’ve ever met,” said Kendra Storm, DNP. “It didn’t matter who you were — what walk of life you came from — she accepted you, and she wanted to do what she could to help you.” Kendra worked alongside Dr. Raymond for over 20 years. “When I lost her, I lost my best friend, my sister, my mentor. I wouldn’t be who I am today without her,” she said.
Dr. Raymond was a special person, a one-of-a-kind combination of leadership, devotion and an unwavering sense of love. “She was the whole package; she was kind, intelligent. She would give you everything,” Kendra said. “She had no idea how wonderful she was. She didn’t know how good she was. For her, it’s just what you do — you go in and take good care of patients.”
Human Value
“If you told her how wonderful this program is because of her, she’d have brushed it off — she’d say this is just what you’re supposed to do,” Kendra said.
“She changed a community,” Dr. Police said. “It’s rare in medicine to see one physician making that big of a difference.” With breast cancer being as common as it is, it’s comforting to know that a program like the one championed by Dr. Raymond exists and is continuing — and not just the distinction of it, but the heart of it, too. “We treat everyone from homeless people to wealthy ranchers,” Dr. Police said, “and we treat everyone — regardless of background — with the same human value.” That sort of unconditional love is the Julie Raymond way.
With all of her heart
Kendra, reminiscing about her friend and mentor, summed up the unforgettable Dr. Raymond, “If a patient needed a commode at their house or a shower chair, she would go and make sure that they had it. If she had a patient call in who couldn’t make it to their appointment, she would go and visit them at their house. She once opened the clinic by herself in the middle of snow storm to meet with patients. She never thought of herself, she only ever thought of others.”
The central theme of the Julie Raymond story is love, and that permeated every setting she was in. “Her family meant the world to her,” Kendra shared. Dr. Raymond’s three kids and her husband were the delight of her life. “She would do anything for them. She loved them with all
of her heart.”
Alice Police, M.D., FACS, (left) is a breast surgeon with more than 25 years of experience. She joined Monument Health after Dr. Raymond’s passing. She works with Kendra to continue the outstanding breast care that is offered at the Cancer Care Institute.
Kendra Storm, DNP, (right) worked alongside Dr. Raymond for over 20 years as her nurse. She credits Dr. Raymond with helping her to pursue excellence and compassion in every way in both her career and life.
Written by Stephen Simpson
Sam, 15, is the kind of guy with whom you want to be friends. He’s smart, cheerful and fun to be around. He’s an athlete, a good student and just an all-around good dude known for wearing fun, silly socks. He’s the kind of person who people support when he needs it. Like in March 2022, when students and staff at Douglas High School all sported crazy socks to show support for Sam and his family.
Why the support? On March 5, 2022, Sam was seriously injured in a car accident. “I don’t really remember it. I know that I had a TBI — a traumatic brain injury,” he explained. “I also had a bruised lung, which was from wearing my seatbelt.” Sam recognized the severity of his injuries, but was quick to clarify, “wearing my seatbelt saved my life.”
Sam, who doesn’t even remember getting in the car that morning, had to be extricated from the vehicle by firefighters. He was rushed to the Rapid City Hospital Emergency Room, and his parents and brother were quick to join him there. The ER physician met with Stacey and Terry Biberdorf, Sam’s mother and father, along with a surgeon. Sam was still unconscious at the time, and both physicians wanted to get diagnostic imaging taken to better understand the injuries Sam had sustained.
Brace for it
“The doctors wanted to do a CAT scan, but Sam had a mouthful of braces at the time, which prevented them from doing it,” said Stacey, Sam’s mom. “When Sam was admitted, his orthodontist actually made a trip to the hospital and removed the braces for us.”
CAT scans and MRIs revealed what Sam’s care team suspected — his unconsciousness was the result of a traumatic brain injury. “At that point, it was just a waiting game to see if and when he would wake up and walk around,” Stacey said.
“We didn’t know what to make of anything,” explained Sam’s dad, Terry. “There’s the fear of the unknown, and you worry if he’s going to wake up.” Stacey added, “but we had fantastic doctors and nurses who helped try to work through everything.”
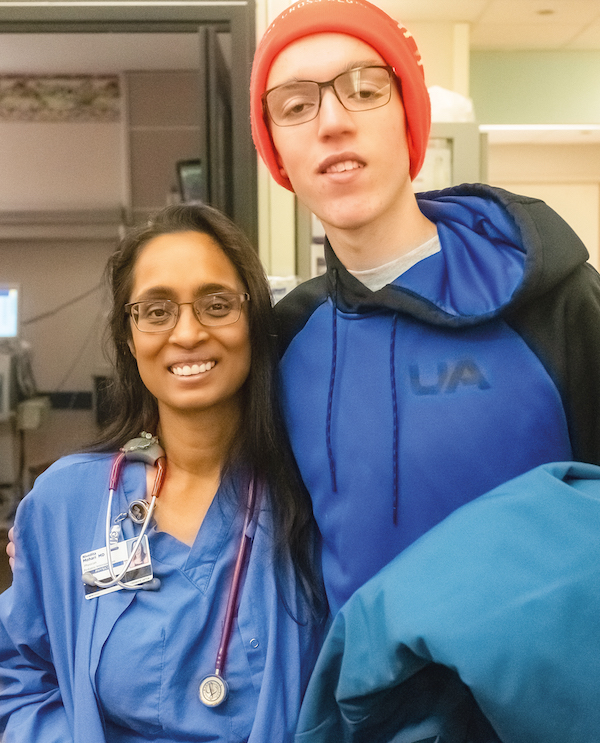 Sam and his family are especially grateful for Nivedita Mohari, M.D., and how she went above and beyond in her care. From advocating for Sam to spend time outside — where he first opened his eyes — to taking great care to coordinate with physicians at Madonna to make his transfer as seamless as possible, the Biberdorfs felt that Dr. Mohari looked after Sam as if he was her own child.
Sam and his family are especially grateful for Nivedita Mohari, M.D., and how she went above and beyond in her care. From advocating for Sam to spend time outside — where he first opened his eyes — to taking great care to coordinate with physicians at Madonna to make his transfer as seamless as possible, the Biberdorfs felt that Dr. Mohari looked after Sam as if he was her own child.
Fresh Air
The Biberdorfs have nothing but praise for Sam’s care team, but for Stacey, one physician stands out — Nivedita Mohari, M.D. Dr. Mohari is an Advanced Care Pediatrics locum Intensivist. A locum is a physician that temporarily works in a practice — a clinic or hospital — that is not their own.
“She always advocated for Sam, even pushing for things that may have raised some eyebrows, like taking him outside. She said, ‘He’s a kid, he’s used to running outside, he needs to be outside, so we’re taking him outside to get some fresh air.’ And that’s when Sam first opened his eyes, when he was outside.”
Sam’s road to recovery wasn’t an easy one. Because of his TBI, Sam couldn’t function normally during his 11-day stay at Rapid City Hospital. This extended beyond lack of consciousness — he couldn’t regulate his temperature and would sweat constantly. Though he wasn’t awake, he was moving constantly, which caused problems with his feeding tube
that actually required surgery to rectify.
Once Sam had opened his eyes and EEGs verified that he was experiencing brain activity, he was transferred to the Madonna Rehabilitation Hospital Lincoln Campus in Lincoln, Neb. Dr. Mohari had worked with physicians at Madonna to begin administering medication before the transfer.
“Through everything, Sam’s nurses were amazing,” Stacey said. “They did so much for him from when he was admitted to when he was transferred, that I can’t even begin to express my thanks.”
Relentless
Sam got right to work once he arrived at Madonna. They immediately evaluated him for occupational, physical and speech therapy. Things were looking up. Stacey said, “As Sam was doing his OT evaluation and was playing a game with his brother, he said his first words since the accident — ‘I win.’”
The physical therapist made it a priority to get Sam out of his wheelchair and moving. “They pushed me really hard, and it was a lot of work,” Sam explained. “I had PT, OT and speech therapy twice a day.” Sam also met with a physician at least once a day to see how things were going and to assess his progress.
“He progressed very fast,” Stacey said.
Sam had to relearn everything: how to speak, how to eat and how to walk and talk. Everything he knew was still in his mind, but he had to learn how to access the information, knowledge and skills all over again. That would be an intimidating task for anyone, but Sam was relentless, coming up with a motto that served him for every step of his rehabilitation.
“I can, I will. Watch me.”
Watch him
Sam’s positive attitude and relentless effort paid off. He was discharged from Madonna and returned to Rapid City, where he continued his rehabilitation via outpatient therapy at Monument Health Orthopedics and Specialty Hospital. Here, he continued to work hard at recovery, quickly completing speech therapy and continuing his occupational therapy and physical therapy.
While Sam was still in Nebraska, he was able to begin working on school work. Physicians told the Biberdorfs that Sam hadn’t lost anything he had previously known — it would just take some time and effort to bring that information to the surface. “Sam has always been an A-plus student, and school is super important to him,” Stacey said.
Returning to school turned out to be a great move for Sam. He continued his outpatient rehabilitation, working on some balance and vision issues related to his traumatic brain injury, but he improved every day. Despite early worries, the young man proved to be the same old Sam, with the same great sense of humor, the same drive, the same positive attitude and the same penchant for wearing silly socks. “Oh yeah, still wearing silly socks,” Sam laughed when asked. “Right now I’m wearing a pair with apes on them.”
It has been a long road to recovery, and Sam still has more to do, but his positive attitude helps him continue to progress. “I’m feeling great,” he said enthusiastically eight months after the accident. “I’m doing all the things I normally do — running, lifting, homework, school and working. As far as running goes, I’m not to the point I was at before the accident, but it all takes time.
I’ll be back there soon enough. I can, I will. Watch me.”
Written by Wade Ellett Photos by Bob Slocum
Rajesh Pradhan, M.D., FACC
My Role
I’ve been the director of cardiovascular imaging since 2016. I’m one of the invasive non-interventional cardiologists in the group. As the cardiovascular imaging director, my job is to oversee running the echocardiology lab, the stress lab, the nuclear stress tests, cardiac CT and all other imaging modalities such as vascular ultrasound. Since I took over the cardiovascular imaging director position, we have brought a lot of new imaging modalities to Rapid City including 3D echocardiology, which has become a central part of the structural cardiac interventions at Monument Health. We also have been working hard to get cardiac CTA to the highest possible quality. Cardiac CTA is a heart imaging test that can help identify severely obstructive coronary disease in patients with symptoms.
My Goal
The number one goal for me is to provide the highest quality patient care. When we go to medical school, we take the Hippocratic Oath, which says that I will put my patient at the center and everything I do will be for the care of my patient. To be able to provide the highest possible care for a patient is my goal. It is also important to me to act as a role model — demonstrating good work-life balance, healthy stress management and working smarter.
My Passion
I love taking care of patients with valve disease. With my training in cardiac imaging, I feel like I've built quite a bit of expertise in that field. Structural interventional cardiology at Monument Health has taken off, and advanced imaging, including interventional echocardiography, assists in those procedures. My colleague, Dr. Purushottam calls me GPS, because I help guide the interventional cardiologists during minimally invasive procedures, such as those to treat valve disease. Interventional echocardiology is a new and rapidly evolving field in cardiology, and along with other cardiologists on the team, we’ve built a successful program here at Monument Health. My other passion is teaching and helping the entire cardiology team be efficient in their work.
Wesley Badger, M.D.
General Surgeon, Spearfish Clinic, North Avenue
People come to Spearfish, S.D. for the outdoors, but General Surgeon, Wesley Badger, M.D., wants to help grow the city into a surgical destination for excellent care. How? By providing high-quality care in the same manner he would like to receive it.
My Role
I am a general surgeon in Spearfish, where I provide broad-based care in the full breadth of general surgery. I was once told that general surgery is the surgery of the skin and its contents. While this may be a bit of an exaggeration, it’s pretty close!
My Goal
Providing care in a small community is such a privilege. The people who we care for are not strangers or nameless faces in a crowd; these are our neighbors, friends or family. My goal is to provide exceptional care to my community.
My Passion
I am passionate about growing Spearfish into a surgical destination for excellent care. I have two separate areas of interest within general surgery. The first is surgery of the thyroid and parathyroid. The second is the management of common bile duct stones through surgical and endoscopic means. The ability to provide these services within our community means that care can be rendered closer to home, when in the past these patients may have needed to be transferred to a higher level of care.
Dr. Badger said that when he sees patients for surgical emergencies in the emergency department or for frightening surgery problems in the clinic, he strives to provide them with a sense of calm. “It is easy to forget that, while this is our day to day, this is a life-changing experience for our patients. I hope to provide care in the same manner that I would wish to receive it.”
My Role
Nurse case managers assess all patients in the inpatient setting to ensure they move smoothly across the continuum of care. As they move from emergency care to more long-term treatment, we create and update their care plan. As a lead case manager, I serve as a resource, advisor and mentor to the case management team, which includes RNs, social workers, case management assistants and transportation coordinators. My role includes partnering with hospitalists to serve as a liaison and resource. I also collaborate with the interdisciplinary care team to help patients and families understand why they are admitted and what their plan of care is while hospitalized as well as coordinate a safe discharge plan.

My Goal
I strive to help every patient have a safe discharge, as well as guide them through complex medical decisions. My hope is that we can improve their quality of life and their success outside of the hospital. As a lead case manager, it is important to me to inspire my teammates through mentoring so they can develop their skills and we can positively impact as many patients and families as possible.
My Passion
Being a patient advocate is something I’m extremely passionate about. I find value in being able to support patients and families through stressful situations by listening to them, understanding their point of view and outlining the next steps so the process seems more manageable.
Case Management is a patient-centered partnership that extends across the continuum of care. Identifying any non-medical factors that influence the patient’s health, recognizing their autonomy and understanding their goals of care are at the center of this work. Case Management works with physicians and the multidisciplinary team to develop a plan that is safe, efficient and cost-effective.
Monument Health is fortunate to have Case Managers with expertise throughout the system such as Sara Snow, who is the Sturgis Hospital Case Manager, and Kim Jenson, who serves our patients on the ambulatory Case Management team.
Growing up, a lot of young people have posters on their walls of athletes and individuals they idolize. They dream of competing with them some day, and in that way, James Carter is living the dream. In the past decade, he’s competed in the same motocross competitions alongside athletes that had previously adorned his childhood walls.
“I’ve been doing freestyle motocross since 2008, and if you’re not super familiar with the sport, it’s basically any type of trick on a dirt bike,” James explained cheerfully. “So that’s anything from backflips to hanging off the bike at 35 feet in the air across a 75-foot gap.” The smile on his face makes it obvious that he loves what he does.
In 2020, James signed a sports performance agreement with Monument Health Sports Performance Institute. He said, “My partnership with Monument Health is one of the biggest accomplishments I have had in my career. I knew I could expect the best health care and great physical therapy — everything I could ask for to know my health would be at 100 percent, which is key for a successful athlete.”
Having ridden, and placed first, in competitions around the globe, and securing sponsorship doing what he loves, it wouldn’t be a stretch to say that James is living the dream.
But living the dream isn’t easy — it takes a lot of hard work and sacrifice to become a professional freestyle motocross legend, and sometimes the best of dreams have moments out of nightmares. That’s something James understands all too well.
James Carter is a professional freestyle motocross athlete who has performed in shows and contests around the globe. This includes the X Games, Nitro Circus World Games, Masters of Dirt and Red Bull X Fighters. As a Monument Health sponsored athlete, James has access to all the training areas at Monument Health Sports Performance Institute powered by exos, and the specialists that work there.
“You know, I wasn’t planning on a sponsorship for me as a rider — I reached out to Monument Health because I was looking for sponsors for the DeadwoodMoto show. I connected with the right people, and I was grateful that Monument Health did sponsor the event. Right after, we had a meeting, and one of the things we talked about was sponsoring me as an athlete, which has been a relationship that I’m really grateful for,” said James.
“If you’re wanting to meet and exceed your goals as an athlete, this place and these people will help you do it.”

The crash
“The last year has probably been one of the wildest times in my life,” James said. “I went from being 32 years old, feeling the best I’ve ever felt and performing the best I ever have, to all of a sudden having an accident — something that seemed, at first, so small compared to everything I’ve done — that turned out to be pretty devastating,” he explained.
James was in Massachusetts when he had the accident, riding a full course at his friend’s property. He took a run at a newly built jump, but it didn’t go as planned. “I over-jumped the first jump, which put me in the face of the next jump,” he said. “I hit my face on the handlebars, and you tend to lose all control after that. You get pushed toward the back of the seat, and it’s a little hard to explain, but your wrist moves down and gives you a bit of a wispy throttle on the next jump.”
Unfortunately for James, the next jump was even more aggressive. He was thrown 30 feet in the air across an 80-foot gap, flying off the bike at its apex, then landing on the backside knuckle — the spot where the landing area meets the downward slope of the ground — on his elbows and knees.
James immediately, and correctly, suspected that he had broken his left femur — he had broken his right femur in 2012 and this felt similar to him. What he first believed to be a dislocated shoulder turned out to be a fractured humerus on his right side. “I knew right away that something bad was going on. We called an ambulance and went straight to the emergency room.”
Hospitalization
To fully recover from his injuries and get back on the bike, James would need to commit to physical therapy. As a Monument Health-sponsored athlete, he knew that excellent physical therapists were ready to help at Monument Health Sports Performance Institute powered by exos, but there was just one problem: James was trapped in a hospital in Massachusetts as the COVID-19 pandemic began wreaking havoc on health care across the country.
Things went from bad to worse. James developed a deep vein thrombosis, a blood clot that often occurs in patients with broken femurs, and then contracted COVID-19 while in the hospital. Despite his condition, he struggled to get any information from his physicians and care team.
“I just didn’t feel like the health care workers there were on my side, and I never had a doctor ever come in and tell me what was going on,” he said with a sigh. “Of course, I was concerned about my future, from the perspective of my health as well as my career. All I really wanted to do was get home, because I knew I’d be in better hands at Monument Health.”
Travel restrictions made that difficult, and even after he had recovered from COVID-19, his blood clot meant James couldn’t fly. The solution to that problem was to rent an RV and drive from Boston to Rapid City. “Luckily I had my buddy Zac Meier, who is also my photographer, who had come out with me to get footage, and he stuck around. My dad also flew out, and the two of them took turns driving straight through.”
“I tried to lay in the back of the RV, and riding in those things is not soft at all,” James continued. “I bounced around and then finally had to move to the front on the couch and just lay there the whole time. It wasn’t an easy trip, but I was so grateful to be home with my daughter, wife, my friends and doctors I knew I could count on.”
Rounding the corner
Returning to South Dakota was a turning point for James. Reunited with family and friends, he began feeling more secure in his future. “Once we got back here, got situated and I talked to Dr. (Daniel) Lochmann, I started to feel a whole lot better about everything,” James said. “He made me feel so much more confident about the prospect of coming back and riding again, although I’ll admit that I definitely thought it wouldn’t take as long as it did.”
Even before his fractures healed, physical therapists at Monument Health got him started on the road to recovery. “When I first saw James, he was still pretty fresh off the accident. He was still using a crutch and had the sling on his right arm,” said Codi Grable, PT. “We started by focusing on basic range of motion, pain control, getting some of his muscles firing again and just getting back to normal day-to-day function and mobility.”
As James made progress, Codi began focusing on higher level strength and getting James into some one-on-one training at Sports Performance Institute. She said it seemed easier to get started with strength in the lower extremities, and then move on to higher-level plyometric exercises with his upper body.
“It was important that we train him to be able to handle the impact of the bike landing, to be able to retain control and not have his hands fall off the bars or anything like that,” Codi said. To help with this, Codi had James do blood flow restriction training, or BFR, which essentially uses a dynamic blood pressure cuff to reduce blood flow to an area. “This tricks your muscles into thinking they’re doing more work than they are,” Codi said. “It allowed us to rebuild some of James’ muscle mass without over-stressing the fracture sites.”
Bryan Olson, PT, also used dry needling to help relieve some pain and tenderness in the injured extremities. Dry needling is a treatment in which a thin needle is pushed through the skin into underlying trigger points in muscle tissue. It may sound a little painful, but is usually only mildly uncomfortable and can relieve a lot of muscle tension and pain.
When Codi went on leave, Bryan also stepped in to help James take the next steps in his rehabilitation. “I got to come in and start working on high-level activities with James, building greater strength in the shoulder and leg and trying to challenge him more in a plyometric capacity, just trying to get him ready for the demands he would face freestyling on the bike.”
Into the gym and beyond
As physical therapy progressed, James was ready to start working with Performance Coach Chris Hathaway at Monument Health Sports Performance Institute powered by exos. “My training with Chris focused on really getting me even stronger than I was before, not just being okay,” James said. “The whole idea was how to make me better on the bike, and I’ll admit that there were days that I hated it. Of course, by the end of the week I would feel better, then the following week, Chris would change it up and I’d be at it again.”
Chris enjoyed working with James because he brought his drive to every session. “There are days he didn’t want to be there — which happens to everyone who trains,” Chris said. “Everybody has days where they would rather stay in bed, but James never let anything stop him. I think he’s been successful at rehabilitation and training for the same reason he has been successful on the back of the dirt bike. He’s got an unstoppable positive attitude.”
Back on the bike — and beyond
After six months of physical therapy and training, it was time for the ultimate test: getting back on the bike. “Throughout my training and rehabilitation, I had one thing in mind, which was, ‘No matter what, I’m riding the September DeadwoodMoto show,’” James said.
He felt ready, but when it came time to practice, he found himself taking a lot of runs toward the ramp, but not taking the jump. “I took about 30 runs before I finally made the jump, and of course afterward I was smacking myself in the head for overthinking and stressing about it,” James said with a quiet chuckle. “Even so, I could tell my shoulder wasn’t as strong as it should be, and I knew I needed to take it easy.”
James rode during that show, and though he wanted to push himself, he exercised caution and protected his shoulder. He did the same at a show the following weekend in Rapid City. He said, “I felt even better at that show, but still I felt like my shoulder wasn’t where it needed to be, and felt like if I had grabbed with just my right arm it might have dislocated.”
Returning to physical therapy the following week, Bryan began working on new ways to focus on that rotator cuff to build more strength into the shoulder. “I’m feeling good again, and I’m still fired up about riding. Now I just want to make sure that I’m doing the right shows.”
For James, the right shows are here in South Dakota, or close enough that he doesn’t have to spend much time away from his family. “My priorities have changed a bit, and the accident is only part of that,” he explained. “I can’t see a future where I’m not riding, but from now on I want to focus on being near my family and doing fun stuff on the bike locally.”
Although James plans on staying on his bike as long as possible, he does plan for when his professional riding days are over. That’s one of the reasons that he’s turned into an entrepreneur, opening B21 Storage in 2022. He has also partnered with his friend Zac to start Wide Open Brew Coffee Co. Their coffee is available online, and they now have an enclosed trailer that converts to a merchandise stand that will sell coffee at races and events in the future.
Additionally, he’s working on ways to help kids who are getting into motocross or other motorsports, through collaborations and potential sponsorships. “I think getting kids on two wheels can make a world of a difference in their lives, just like it did in mine.”
“I don’t know exactly what will come next for me,” James said, smiling playfully. “But I’m addicted to cars, motorcycles and coffee, so you can bet they’ll be involved.”
Functional Dry Needling (FDN) is a technique used to treat dysfunction in neural, muscular or connective tissue, by inserting an extremely thin but solid needle into muscular trigger points. Dry Needling can be used to treat acute injury, chronic disease process, overuse syndromes/injuries, post-surgical diagnoses and more. Therapists at Monument Health use FDN as one part of a comprehensive approach to help improve, restore and optimize movement and function.
Dry Needling can result in:
• Increased blood flow
• Decreased pain and inflammation
• Deactivation of the trigger point
• Normalization of muscle tone

James said he felt like he was in good hands with both Codi and Bryan, because they’re both familiar with the demands of motocross. Bryan’s nephew races motocross, so he had an idea of what James would need. “There’s a lot of demands on the body when you’re doing that kind of riding,” Bryan said. “James has to control the bike and his body, while he’s riding, while in the air and then through the landing. Pain and limited mobility can really throw off that timing.”
Codi has an even better understanding of motocross. “I grew up watching motocross, and then I ended up marrying a motocross rider,” she said with a laugh. “He raced for a long time, and his family runs the 4Gmx Indoor Motocross series. Racing and freestyle are different, but if you’re familiar with one you’re familiar with the other.”
“James sustained severe long bone fractures to femur and humerus, both requiring extensive reconstruction. This was also complicated by a pulmonary embolism and COVID-19, increasing his risk of complications and need for further surgery. He had his surgery in Boston, but was able to be transferred home within a week of the accident.
He was always extremely motivated and cooperative with his rehab and recovery restrictions, needing mostly to be reminded not to be doing ‘too much.’ At one year, he is still in rehab, working to get back on his motorcycle. I wouldn’t recommend getting back on the bike too quickly, but with his ambition, it’s difficult to slow him down.”
Daniel Lochmann, M.D.
Written by Wade Ellett Photos by Bob Slocum & Zac Meier
Blood Flow Restriction (BFR) Training is a specialized treatment involving restricting circulation in an extremity while exercising at a light intensity. Despite the light intensity, exercising in this state stimulates significant responses that mimic exercising with much higher loads. This causes strength and conditioning gains, as well as supporting an accelerated healing response, that would normally require a much more intensive workout routine.
Benefits of BFR Training include:
• Accelerated soft tissue and bone healing responses.
• Applicable to patients that have limited weight-bearing ability or other limitations.
• Increased repair of muscle tissue, gains in muscular strength and improvements in overall endurance.
My Role
I see to the nonclinical needs of our patients and their loved ones while they are waiting to see a doctor in the emergency room. I guide a patient’s support person to the right rooms, help guests find their way around, provide comfort or distraction items or simply offer a listening ear when it’s needed. I also help people find services outside the hospital, such as contact information for taxis, hotels and pharmacies, among many other things.
My Goal
My goal is to provide an informative and caring environment for our hospital’s guests and make them as comfortable as I can while they wait. I want to provide comfort to our guests, even if it is just for a few moments. A personal goal of mine
is to expand my knowledge base and further my education.
My Passion
I strive to help our patients and guests emotionally who may be in a state of panic, pain or anxiety. We come in and give that little extra love and attention to the patients and their guests to make them more comfortable. I find that rewarding.
Monument Health Guest Services provides a welcoming atmosphere and promotes a patient- and family-centered approach to care. These caregivers offer a variety of vital, nonclinical services that include helping guests find their way around the hospital and providing patients and their guests with important information, support resources and programs. The services offered range from welcoming people as they enter the hospital to parking guest vehicles.
My Role
I have a variety of roles at Monument Health. The first is in the Intensive Care Unit where I care for some of our sickest patients. The ICU tends to be fast paced and usually requires cooperative care with multiple other specialties. When I’m not in the ICU, I can usually be found either in the clinic or the hospital taking care of pulmonary patients. Pulmonary medicine has a different flavor of care, often with patients with more chronic and complex diseases like COPD and pulmonary fibrosis. Lastly, I’m the Medical Director for Respiratory Therapy. Our respiratory therapists are crucial for taking care of all of our patients with respiratory disease.
My Goal
My goal is always to help patients and families navigate through their illnesses. Sometimes that’s accomplished directly through my care of the patient; other times it may be as part of the team, or making sure the patient gets connected to the right services. Part of that goal has been to expand our pulmonary services in order to ensure the Black Hills continues having access to high-quality pulmonary care. In the last few years, that has included developing our EBUS program, and more recently an addition of robotic navigational bronchoscopy with the ION system. Both of these help with our pulmonary diagnostics, particularly in the area of llung cancer.
My Passion
My passion, as it relates to being a physician, is making a difference. That may be as simple as prescribing a medicine for a patient so they can breathe easier or listening to a patient’s stresses in an effort to alleviate them. It may be more complex, like helping to launch an ION program so that patients with lung cancer can get their diagnosis and staging more efficiently and get to treatment faster. As a physician, I feel I have a responsibility to try to make life better for my patients, my coworkers and my community. Ultimately making an impact, great or small, in people’s lives gives me great joy.
My Role
I am a general orthopedic surgeon, so I evaluate and diagnose complaints involving the musculoskeletal system, come up with a treatment plan and help patients move and feel better through surgery and collaboration with other orthopedic specialists. I focus largely on pediatric orthopedics, trauma, hand, and hip and knee replacement.
My Goal
I provide a caring experience to adults and kids requiring orthopedic services in the Black Hills. I’m also excited to provide outreach orthopedic services to Monument Health Custer and Hot Springs clinics. I always aim to provide the highest-quality care possible, so that my patients have less pain and can return to active lifestyles doing things that they enjoy.
My Passion
I enjoy serving my community. I am passionate about serving my patients and I want them to know that I am willing to do the work to get them back to living their full lives. Being able to work with a variety of patients in our area is such an incredible opportunity. Outside of work, I love spending time traveling, reading, hiking and practicing yoga.
At Monument Health, you’ll receive high-quality care by a board-certified orthopedic surgeon and a comprehensive team of trained orthopedic specialists. With our years of experience, we are proud to offer a fast track of comprehensive care with services such as same-day total joint replacement focused on getting you back home again.
What is the Monument Health Veterans Group?
We are a group of 322 veterans who are also physicians and caregivers working at Monument Health. We make up a volunteer group to support our patients and communities. Our main goal is making connections with veterans who are being treated at our inpatient facilities. When registering, veterans can request a visit by one of our volunteers, and we do our best to make it happen.
Why is it so important that this group exists at Monument Health?
There are a significant number of veterans living in the communities we serve, many of them work for Monument Health. Because of that, we go the extra mile to show our veteran patients and communities how much we care about them. Military service provides a unique perspective, and veterans often share an unspoken bond from experiences that are hard to understand if you haven’t lived through them. That shared understanding — knowing you’re not alone — can have a major impact on patient care.
What are some of the goals and projects that the Military Veterans Group has completed?
We provide Hero Walks, which is when a veteran passes away, we line the hallway to pay our respects to them and to their family. We try to provide veteran inpatients with a visit when requested and place a branch-related veteran magnet and an American flag magnet on the frame of their room door. We also present them with a pin and certificate, thanking them for their service. Volunteering is a big part of our group. We’re always looking for opportunitiesat veteran-related events throughout the Black Hills.
What would you like people to know about the group?
Every one of our members has volunteered in caring for veterans and their families during critical times in their lives. This spirit of service is strengthened by the sisterhood and brotherhood we share as former service members.
What is your role at Monument Health?
I am a Certified Pharmacy Technician at Lead-Deadwood Hospital.
Who do you volunteer with, and why?
I help several local charities by organizing and running an annual community rummage sale. It started as a one-off event, but it was so successful we decided to keep running it every year. The proceeds from the rummage sale go to organizations in Lawrence County like City Clothing Center — also known as the “free store” — Lord’s Cupboard and Boys & Girls Club of the Black Hills.
Why do you think it’s important to give back to the community?
Helping charities helps others. Our communities are our homes, and nonprofits are an important part of that. Even by helping in small ways, we can make a big difference in the lives of others. Helping local charitable organizations is paying it forward in our communities.
How do you think volunteering makes you a better caregiver?
Volunteering keeps me grounded and helps keep the compassion real. Sometimes it’s easy for me to get caught up in the stresses of everyday work and life, but then seeing a big smile on the face of someone I’ve helped — that’s what makes life real.
“Death is very difficult to talk about. I recognized that very early in my grief,” said Bri Edwards, a Physician Assistant in General Surgery at Monument Health. “People don’t know what to do or to say.”
Her son, Lachlan, was born in 2007. “His smile would light up a room,” she said. In 2008, at 10 and a half months, Lachlan didn’t wake up from his nap. He had died from SIDS. Bri was a mom who wanted answers. What she found was a sacred duty to tell her story and to walk alongside other moms and dads who are experiencing the darkest nights of parenthood.
‘Like a Thousand Pounds on Your Chest’
“SIDS is a diagnosis of exclusion,” Bri explained. That means when all other causes of death are ruled out, examiners label the baby’s death certificate with sudden infant death syndrome, or SIDS. This label leaves around 3,500 families in the U.S. each year with few answers following an unimaginable tragedy.
The grieving process surrounding the unexpected loss of a baby is unique to each parent, but there are elements to that season of loss that are consistent. “The illustration that I use a lot when I’m walking grieving parents through this is that it feels like a thousand pounds being dropped on your chest,” Bri said. “You can’t breathe, you can’t think. It seems like you’ll never be able to experience joy ever again.”
The numbness, the rage and the despair that families experience in the wake of SIDS can seem endless. “But being able to see another family experience joy after a loss can be the start of rebuilding hope,” she said.
Sudden Infant Death Syndrome
The exact cause of SIDS remains unknown to researchers, but effective ways to reduce the risk of unexpected infant death are clear. One of the most important practices parents/caregivers can observe is safe sleep. Safe sleep practices were established and promoted starting in the 1990s. Research shows this push for safe sleep has led to a decline of SIDS deaths from 130.3 deaths per 100,000 live births in 1990 to 38.4 deaths per 100,000 live births in 2020.
A Legacy of Hope
 At the time of Lachlan’s death, Bri and her husband were reeling and found themselves in a desperate search for help and resources. “We couldn’t find anything in South Dakota,” she said. So, Bri decided to start her own way to support parents experiencing grief from the unexpected loss of a child.
At the time of Lachlan’s death, Bri and her husband were reeling and found themselves in a desperate search for help and resources. “We couldn’t find anything in South Dakota,” she said. So, Bri decided to start her own way to support parents experiencing grief from the unexpected loss of a child.
Lach’s Legacy was born. Bri’s organization offers connection, comfort and hope to families in South Dakota experiencing the loss of a child. “We’ve been able to send over 100 care packages to families in their early days of grief,” Bri said
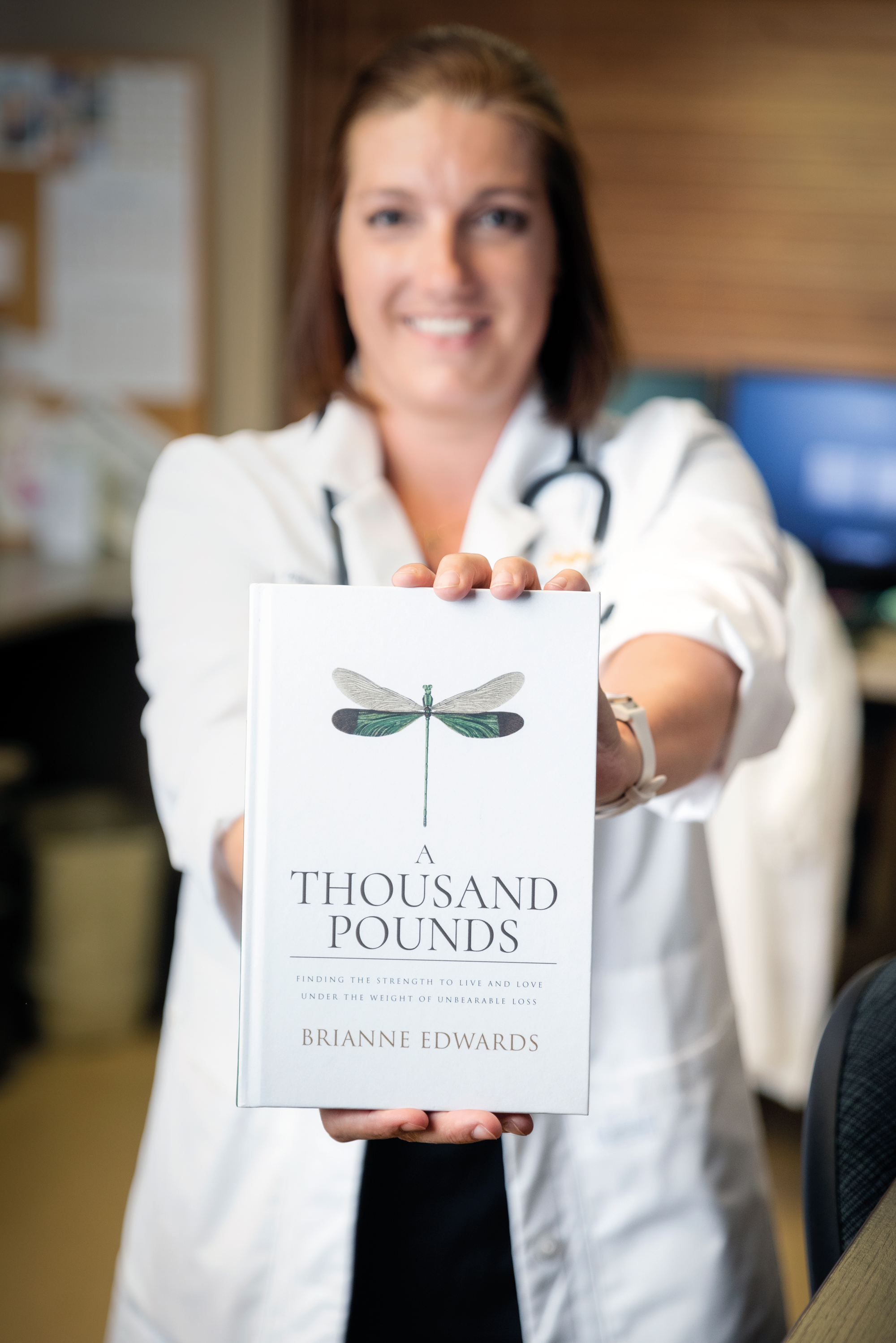 Lach’s Legacy is a nonprofit organization dedicated to the fight against SIDS and other sleep-related infant deaths in South Dakota. The organization offers connections, comfort and hope for those grieving the loss of an infant.
Lach’s Legacy is a nonprofit organization dedicated to the fight against SIDS and other sleep-related infant deaths in South Dakota. The organization offers connections, comfort and hope for those grieving the loss of an infant.
Brianne Edwards started Lach’s Legacy to help families who are experiencing the unexpected loss of a baby. The newest facet of Lach’s Legacy is available now in the form of a book on coping with grief, A Thousand Pounds: Finding the Strength to Live and Love under the Weight of Unbearable Loss. Bri wrote this book to help grieving parents discover their own journey by guiding them through hers.
In addition to helping families navigate the death of a daughter or son, Lach’s Legacy has been able to contribute to the fight against SIDS by raising over $40,000 for research. Bri and her team are also helping to spread the word on best practices for parents to reduce the risk of SIDS. “We, first, work to prevent families from ever having to experience this tragedy. Second, to provide a warm embrace of comfort in the wake of the unimaginable.”
Lachlan was only in his parents’ arms for 10-and-a-half-months, but he’ll always be with his mom and dad. Every time Lach’s family comforts another family following the unexpected loss of a baby, Lach — in a way — is offering that hug or that listening ear, too.
Here are five things parents need to know about safe sleep:
- Place babies on their backs for naps and bedtime.
- Use a firm mattress with tight fitting sheets in a safety-approved crib or bassinet for baby’s sleep.
- Keep loose items out of the baby’s crib — no crib bumpers, stuffed animals, blankets or other loose items.
- New babies should share a bedroom with their parents, but not the bed itself.
- Look for signs of the baby overheating like sweating or being hot to the touch.
As the Hippocratic Oath states, “There is art to medicine as well as science.” This oath sworn by many physicians goes on to state that, “Warmth, sympathy and understanding may outweigh the surgeon’s knife or the chemist’s drug.” No other group of caregivers may understand this balance more than the team behind end-of-life care.
A Special Bond
Caregivers who choose to enter a career in end-of-life care are accepting a special assignment. “We really get to help patients and their families at a really scary time in life,” said Michelle Sieveke, Director of Home Health, Hospice and Palliative Care at Monument Health. Medical strategies in end-of-life care work to treat the whole person through physical, mental and spiritual care.
One of the most important aspects of the hospice philosophy goes beyond the patients themselves. “We’re not only there for the patient; we’re there for the family, as well,” Michelle said. “Families and caregivers get to create a special bond.” Following the passing of a loved one, family members are eligible for up to 12 months of grief support from Monument Health caregivers.
An Extra Drive
Crystal Philpot, the Nurse Manager for Monument Health Home Health and Hospice, shared what it takes to be a caregiver who specializes in end-of-life care. “They have to have an extra drive to connect on a one-on-one basis with patients.” Caregivers who work in hospice, palliative and home care include doctors, nurses, social workers and other specialists who are able to focus on specific aspects of end-of-life care.
“Everyone who starts in this field of health care comes in with an idea of what they think it is,” Crystal said. “They get to see the part they play in a patient passing with dignity and grace. Then they connect the dots of how important and fulfilling what they’re doing is.”
Hospice and Palliative Care
These common terms associated with end-of-life care may seem interchangeable, but each word refers to a unique facet of this field of health care.
Hospice is a philosophy of care that centers around a person who has received a prognosis from their doctor that they have six months or less to live. Hospice care can happen in that person’s home, an assisted living facility or a specialized hospice facility. Curative treatments cease and caregivers focus on comfort and quality of life.
Palliative care is the field of health care that centers on easing the pain and suffering of patients. Palliative care may be included as part of hospice care, but it can also be part of a prognosis that includes curative measures. Caregivers can use palliative medicine and treatments to help their patients, for example, find relief from chronic pain or nausea.
Hospice caregivers are committed to making a lasting difference in the lives of patients diagnosed with a life-limiting illness by enabling them and their loved ones to live each day as fully and as comfortably as possible. Most Hospice patients live in their own home, but Home+ Hospice Care is available for people no matter where they call “home” — a private home, assisted living, nursing home, or the Hospice House. To learn more about the Hospice Care or the Hospice House visit: monument.health/services/hospice.
Memories
“People will always ask me, ‘How can you work in that setting? Isn’t it depressing?’” Crystal said. “To that, I’ll always explain the importance of what we do. When you look back on those really important days in your life, you may not remember the exact details of the moment, but you definitely remember how you felt. And that stays with you forever. My goal is to teach our caregivers that’s what will happen for the loved ones of our patients. You need to provide that experience and that environment so that when the patient’s loved ones look back, it’s a good memory.”
Michelle added, “Our caregivers would say that this is extremely rewarding and fulfilling work.” We are honored to bring a little light to a family’s darkest days and are truly living out a calling to serve our communities.
Whitney Driscoll started biking with an ulterior motive. “I really, really like to ski,” he said. “So, I started mountain biking to stay in shape for skiing.” But as he explored in and around his hometown of Spearfish on the seat of his bike, he started to enjoy the sport for its own charms. To give himself a goal, Whitney started to enter bike races — including the Dakota Five-O, an annual 50-mile mountain bike race.
In December 2020, something started to change for Whitney. “I know the exact spot where I first noticed it. I call it ‘heart attack hill,’” he said. Whitney was riding a gravel trail in the Black Hills when he noticed a strange feeling to the left of his sternum. “It kept happening into January. So, I called my friend who’s a vascular surgeon. He told me I needed to go in and start ruling some very serious things out.” Whitney made an appointment to see his doctor, Jay Bogard, M.D., in Spearfish. Whitney went through a stress test, but it didn’t show any abnormalities.
“After that, my wife and I went down to Arizona,” Whitney said. “We were doing some rides down there that I had done easily before, but it left me feeling wiped out. I finally told my wife that I needed to see the doctor again. So I called Dr. Bogard from Arizona and made an appointment.”
Whitney’s Experience
Dr. Bogard was determined to pinpoint what was causing Whitney’s chest discomfort and fatigue. “I think the phrase he used was ‘full-court press,’” Whitney said. Dr. Bogard discovered that Whitney’s troponin levels were elevated. Troponin is a protein that appears in blood when the heart is damaged. Dr. Bogard then ordered an echocardiogram. The mood changed when Dr. Bogard was able to see Whitney’s heart.
Whitney was then rushed by ambulance to Rapid City for surgery. “I realized how serious it was when the cardiologist, Dr. Heilman, met me at the door of the ER in Rapid City,” Whitney said. Whitney had major blockages in his heart and received a stent.
Following recovery, Whitney found that his support from Monument Health didn’t end. “After I went home, Dr. Bogard and Dr. Heilman took the time to call me — it wasn’t me calling them; they called me,” Whitney explained. “They really helped to find the right balance of medication that worked with my active lifestyle.”
Following his surgery, Whitney returned to mountain biking and skiing. He attributed his speedy return to his exercise routine to the tailored attention he received from his caregivers at Monument Health. “Dr. Bogard has been awesome. He’s super available, whether it’s sending him a quick message on MyChart or giving him a call. The individualized care has been incredible.”
Taking It Seriously
John Heilman, M.D., FACC, Chairman of the Cardiovascular Department at Monument Health and Whitney Driscoll’s cardiologist, points out how his patient’s actions made for a successful experience during his cardiac event.
“Whitney was persistent and advocated for himself,” Dr. Heilman shared. “It’s very important for patients to pay attention to any new or unusual symptoms.” Whitney’s decisive actions contributed to his ultimate recovery. “Some people recognize the seriousness of these symptoms immediately,” Dr. Heilman said.
“Others will have symptoms for months and then seek medical attention. The third group may deny the seriousness of their symptoms and chalk it up to indigestion or a cold.”
Dr. Heilman reminds people not to ignore these and other symptoms:
- Shortness of breath
- Tightness or squeezing sensation in the chest
- Sweating
- Feeling ill at ease
- Nausea
- Pain radiating from the chest to the back, arm or jaw
Ryan’s Experience
A little over a year later, Whitney’s 27-year-old son, Ryan, began experiencing chest discomfort. “I was diagnosed with AVNRT back in eighth grade,” Ryan explained. Atrioventricular nodal reentrant tachycardia causes the heart to beat much faster than normal. To manage the symptoms, people afflicted with AVNRT use different breathing techniques to reduce their heart rate during trachyocartic episodes.
One day, his ability to manage his AVNRT changed. “All of a sudden my breathing techniques weren’t working as well. I couldn’t get my heart to slow down very much,” Ryan said. “I was talking to my dad about it, and he suggested I go see Dr. Bogard. So, I made an appointment.”
When Ryan went to Dr. Bogard’s office in Spearfish, his heart was beating around 200 beats per minute. “I was in Dr. Bogard’s office for about 20 minutes before they sent me to the ER to get my heart rate down,” Ryan said.
Once caregivers at the Spearfish ER were able to slow Ryan’s heart rate, he was taken by ambulance to Rapid City Hospital for surgery. “I remember being really impressed with the new Heart and Vascular Institute. It’s really cool to have access to a facility like that in South Dakota,” Ryan said. “The other thing that really blew me away was how well each team worked and communicated together.”
Ryan’s surgery worked to normalize his heartbeat. “My surgery lasted for three hours. I recovered for a few hours, and I was able to go home around 8 p.m.,” he said.
Both father and son faced unique challenges and in the end were able to walk away from their experiences with new perspectives and grateful attitudes. Whitney has this advice: “If you feel your heart and it’s not feeling quite right, be humble enough to go get yourself checked out.”
Brandi Tackett, Director of Infusion Services at Monument Health, learned early in life that the subject of medicine energizes her. When she was growing up, her grandma had diabetes. She points to this as the beginning of her desire to understand how medication can help people.
“I then spent some time working in a rural health clinic in high school,” she said. “I learned there that I really love the study and the science behind medication.” Brandi didn’t miss a beat pursuing her passion. “I started pharmacy school when I was 17,” she explained.
Getting Excited for Vaccines
One particular topic in medication that gets Brandi buzzing with excitement is vaccines and immunization. “If I could tell people one thing about vaccines, it would be that they are the biggest success story in the history of public health,” she shared. By harnessing the natural response of the immune system, vaccines have changed the well-being of humankind in a way that can’t be overstated. “The World Health Organization did a study recently, and they estimated that about 5 million lives each year are saved thanks to vaccines.” Most of the lives being saved by vaccines belong to children from all over the world.
3 Facts about Vaccines
About 200 years ago, Edward Jenner, a British physician, observed that milkmaids who had been infected with cowpox seemed to be immune to the similar but much deadlier smallpox. Jenner began to experiment with intentionally infecting people with cowpox to protect them from smallpox. Jenner would later name this process vaccination — vacca being Latin for cow.
Children benefit the most from the worldwide spread of vaccines. Every year, vaccines save the lives of about 3 million children. Since 1988, the number of children paralyzed by polio has shrunk by over 99 percent.
Vaccines have come a long way. One of the latest advancements in vaccinology is mRNA vaccines. Instead of infecting the body with a weakened form of the virus, scientists are able to create a protein that instructs cells how to fight off specific diseases. This technology has been in development for decades. The first commercially distributed mRNA vaccine was the vaccine for SARS-CoV-2.
Assemble Your Team
To ensure that you’re making the best decisions for your health, it’s best to speak with an expert. “The medication process can be very complex,” Brandi said. “Make sure you’re bringing a team of people around the medications you use. It’s about asking questions to your doctor, your nurse and your pharmacist.” The caregivers at Monument Health are passionate about helping people make informed and complete decisions about their medication and vaccines.
Brandi makes sure that all of her family and friends are vaccinated against two diseases when they’re eligible for the shots: pneumococcal pneumonia and shingles. “Both of these can have some serious health consequences if you contract them,” she said.
Pneumococcal Vaccine
Pneumococcal disease can cause pneumonia, meningitis, sepsis and other potentially deadly infections. Adults 65 years and older as well as some younger adults who are at risk should get a pneumococcal vaccine. Children under 2 also are eligible for a version of the pneumococcal vaccine. In children, the vaccine significantly reduces the risk of early childhood ailments like ear infections. The complications caused by pneumococcal diseases can range from inconvenient to life-threatening. Aging is complicated enough. If you’re 65 or older, talk to your doctor or pharmacist about the protection that a pneumococcal vaccine can provide.
Shingles Vaccine
Shingles is caused by the same virus that causes chickenpox, the varicella-zoster virus. If you were infected with chickenpox as a child, the virus remains dormant in your body. The virus can reemerge years later as shingles. Although shingles isn’t life-threatening, the infection can result in extremely painful blisters and rashes and may even cause permanent nerve damage and long-term pain. If the shingles rash spreads to the face and eyes, vision loss can occur. Everyone 50 years or older should get the shingles vaccine. This vaccine is administered in two doses with two to six weeks between doses. The potential pain and complications caused by shingles can be reduced by over 90 percent with two simple shots.



.jpg)














.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)
.jpg)

















